Table of Contents
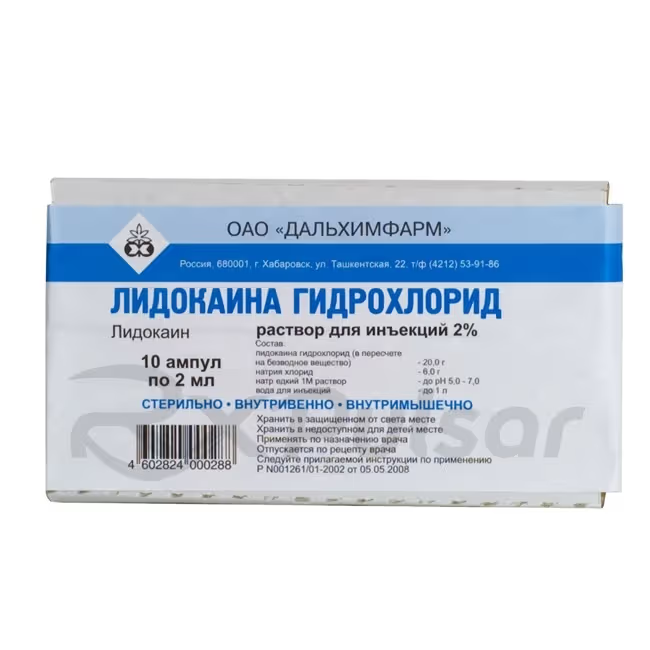
LIDOCAINE 20mg/ml Solution 2ml 10pcs Buy Online
Lidocaine Injection Solution: A Comprehensive Overview
Lidocaine, a widely used medication, plays a crucial role in various medical procedures and treatments. Its efficacy and relative safety profile make it a cornerstone of modern medicine, though understanding its properties and potential side effects is vital.
This overview provides a comprehensive look at lidocaine injection solution, focusing on its mechanism of action, applications, and safety considerations. This information is intended for educational purposes and should not be considered medical advice. Always consult a healthcare professional for any health concerns.
Lidocaine’s versatility makes it indispensable across several medical specialties. Proper administration and awareness of potential complications are paramount to ensuring safe and effective use.
What is Lidocaine?
Lidocaine is a widely used local anesthetic and antiarrhythmic drug. As a local anesthetic, it effectively numbs a specific area of the body by blocking nerve signals responsible for pain and other sensations. This allows for painless medical procedures, such as surgeries and dental work. Its antiarrhythmic properties stem from its ability to stabilize the heart’s rhythm, making it useful in treating certain cardiac conditions.
The mechanism of action involves the blocking of voltage-gated sodium channels in nerve cells. This prevents the transmission of nerve impulses, resulting in the loss of sensation. Importantly, lidocaine’s effects are typically temporary and reversible, wearing off as the drug is metabolized by the body. Different concentrations are used depending on the intended application, with higher concentrations producing deeper and longer-lasting numbness.
Lidocaine is available in various forms, including injection solutions, topical creams, gels, and sprays. The choice of formulation depends on the specific medical need and the area to be treated. Injectable forms, like the 20mg/ml solution, are commonly used for nerve blocks, infiltration anesthesia, and spinal anesthesia during surgical procedures. Its rapid onset of action and relatively short duration make it a versatile tool in a variety of clinical settings. The precise duration depends on the concentration, route of administration and other factors.
Mechanism of Action
Lidocaine’s primary mechanism involves the reversible blockade of voltage-gated sodium channels in nerve cell membranes. These channels are crucial for the propagation of nerve impulses, specifically those responsible for transmitting pain signals. By binding to these channels, lidocaine prevents the influx of sodium ions, thus disrupting the depolarization process necessary for impulse transmission.
This disruption effectively blocks the conduction of nerve impulses, leading to a loss of sensation in the affected area. The degree of blockade depends on factors such as the concentration of lidocaine, the duration of exposure, and the type of nerve fibers involved. Smaller, unmyelinated nerve fibers (responsible for pain and temperature sensation) are typically blocked more readily than larger, myelinated fibers (responsible for touch and pressure).
In its role as an antiarrhythmic agent, lidocaine exerts a similar effect on cardiac sodium channels. This action stabilizes the heart’s electrical activity by suppressing abnormal impulses that trigger arrhythmias. This stabilization prevents the rapid, erratic heartbeats characteristic of certain arrhythmias. The specific effects on the heart are nuanced and are dependent on the concentration and mode of administration.
Uses and Applications
Lidocaine injection solution finds extensive use in various medical settings, primarily as a local anesthetic to alleviate pain during procedures. Its versatility allows for applications ranging from minor surgical interventions to more complex procedures requiring extensive anesthesia. The 20mg/ml concentration is frequently employed for various types of regional anesthesia.
Specific applications include: Infiltration anesthesia, where lidocaine is injected directly into the tissues to numb a specific area before procedures like wound repair or biopsies; nerve block anesthesia, targeting specific nerves to numb larger regions, commonly used in dental procedures or limb surgeries; and spinal or epidural anesthesia, which involves injecting lidocaine into the spinal canal to achieve widespread pain relief during major surgeries.
Beyond its role as a local anesthetic, lidocaine is also used in the management of certain cardiac arrhythmias. Its ability to stabilize the heart’s electrical activity makes it a valuable tool in emergency situations where rapid intervention is required to restore a normal heart rhythm. However, its use in this context is typically limited to acute situations and requires careful monitoring by trained medical professionals. The precise dosage and administration method vary greatly depending on the specific clinical indication.
Pharmacokinetics and Metabolism
Understanding lidocaine’s pharmacokinetic profile is crucial for safe and effective use. After administration, lidocaine is rapidly absorbed into the bloodstream, with the rate of absorption varying depending on the route of administration. Intravenous injection results in the quickest absorption, while intramuscular or subcutaneous injection leads to slower absorption rates. The absorption from topical application is even slower and less predictable.
Distribution throughout the body is also rapid, with lidocaine readily penetrating well-perfused tissues such as the heart, lungs, brain, liver, and kidneys. It also crosses the placental barrier and enters breast milk. The extent of protein binding to plasma proteins (approximately 50-80%) influences the distribution and duration of action. Highly protein-bound lidocaine is less readily available to exert its effects.
Metabolism primarily occurs in the liver via hepatic microsomal enzymes, primarily through N-dealkylation and amide hydrolysis. These metabolic pathways produce metabolites, some of which retain anesthetic activity, albeit to a lesser extent than the parent compound. The elimination half-life is typically 1.5-2 hours, although this can be prolonged in patients with hepatic or renal impairment. Excretion occurs primarily through the kidneys, with a smaller portion eliminated through the bile.
Pros of Lidocaine Injection Solution
Lidocaine injection offers several significant advantages in various medical applications. Its rapid onset of action is a key benefit, providing quick pain relief, crucial during procedures where immediate anesthesia is needed. This rapid onset minimizes patient discomfort and allows for efficient completion of medical interventions. The relatively short duration of action is also advantageous, as it limits prolonged systemic effects.
The effectiveness and reliability of lidocaine in achieving local anesthesia are well-established. It consistently provides effective pain relief across a range of procedures and surgical settings, making it a dependable choice for healthcare professionals. Its efficacy is further enhanced by the potential to combine it with vasoconstrictors, prolonging its anesthetic effects. This combination is particularly beneficial for procedures in highly vascular areas.
Lidocaine’s versatility allows for various administration routes, including infiltration, nerve blocks, and spinal or epidural anesthesia, making it suitable for a wide array of procedures and anatomical locations. This adaptability caters to different clinical needs and patient conditions, offering flexibility in anesthesia management. Additionally, lidocaine generally has a favorable safety profile when administered correctly, with manageable side effects in most patients.
Cons of Lidocaine Injection Solution
Despite its numerous advantages, lidocaine injection also presents some potential drawbacks. One significant concern is the risk of adverse effects, ranging from mild reactions like localized pain or swelling at the injection site to more serious systemic effects such as cardiovascular or neurological toxicity. These risks are generally low when the drug is administered correctly and within recommended dosages, but careful monitoring is crucial.
The duration of action, while sometimes advantageous, can also be a limitation depending on the clinical context. For procedures requiring prolonged anesthesia, repeated injections or the use of longer-acting anesthetics may be necessary. This can increase the risk of cumulative toxicity and necessitates careful attention to dosage limits. The potential for allergic reactions, although uncommon, also represents a contraindication for some patients.
Furthermore, incorrect administration can lead to various complications. Accidental intravascular injection, for instance, can result in rapid absorption and potentially serious systemic effects. Precise injection technique, aspiration to avoid intravascular injection, and careful monitoring of the patient are essential to minimize these risks. The potential for local tissue damage at the injection site is also a factor to consider, although this is largely dependent on technique.
Contraindications and Precautions
Several factors necessitate caution or contraindicate the use of lidocaine injection solution. Pre-existing heart conditions, such as severe bradycardia, heart block, or significant myocardial dysfunction, represent major contraindications due to the potential for worsening cardiac arrhythmias. Patients with a known hypersensitivity or allergy to lidocaine or other amide-type local anesthetics should also avoid its use. A history of seizures or epilepsy requires careful consideration, as lidocaine can lower the seizure threshold.
Patients with impaired liver or kidney function require careful monitoring and potentially dose adjustments due to the altered metabolism and excretion of lidocaine. In such cases, the risk of accumulating toxic levels of the drug is heightened. The use of lidocaine in pregnant or breastfeeding women also warrants careful consideration due to its potential to cross the placental barrier and enter breast milk. The benefits must be carefully weighed against potential risks to the fetus or infant.
Adverse Effects and Management
While generally safe when administered correctly, lidocaine can cause adverse effects. Local reactions at the injection site, such as pain, swelling, or redness, are relatively common and usually mild and transient. More serious adverse effects are less frequent but can include cardiovascular toxicity, manifesting as bradycardia, hypotension, or arrhythmias, and neurological toxicity, such as dizziness, drowsiness, confusion, or seizures. The severity of these effects is largely dose-dependent.
Management of adverse effects depends on their severity. Mild local reactions typically require no specific treatment and resolve spontaneously. More severe reactions, however, necessitate immediate medical intervention. Cardiovascular toxicity may require supportive measures such as intravenous fluids, vasopressors, or antiarrhythmic medications. Neurological toxicity might necessitate treatment with anticonvulsants such as diazepam to control seizures. Prompt recognition and appropriate management are critical to minimizing the risk of serious complications.
Careful monitoring of vital signs, particularly heart rate and blood pressure, is essential during and after lidocaine administration. Patients should be observed for any signs or symptoms of toxicity, and immediate medical attention should be sought if any concerning symptoms arise. Prevention is paramount; adhering to recommended dosages, proper injection techniques, and careful patient selection significantly reduces the likelihood of adverse events. Early intervention is key to mitigating potential adverse outcomes.
Conclusion
Lidocaine injection solution remains a valuable and widely used medication in modern medicine. Its efficacy as a local anesthetic and its utility in managing certain cardiac arrhythmias make it indispensable across various medical specialties. However, understanding its mechanism of action, potential adverse effects, and contraindications is paramount for safe and effective use.
The benefits of lidocaine, particularly its rapid onset and relatively short duration of action, are considerable. Yet, healthcare professionals must carefully weigh these advantages against the potential risks of adverse effects, especially in patients with pre-existing conditions or those taking other medications. Strict adherence to recommended dosages and administration techniques is essential to minimize these risks. Always prioritize patient safety and utilize lidocaine judiciously and under appropriate medical supervision.
Further research continues to explore the applications and refine the understanding of lidocaine’s pharmacodynamics and pharmacokinetics. This ongoing investigation aims to enhance its safety profile and further optimize its therapeutic benefits. The responsible use of lidocaine, guided by up-to-date medical knowledge, remains critical to ensuring its continued effectiveness and minimizing potential harms for patients.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Elizabeth Dennis, MD [Medical reviewer]
Elizabeth Dennis, MD [Medical reviewer]Dr. Elizabeth Dennis is a highly skilled Orthopedic Surgeon and consultant for RxPulsar.com, a licensed online pharmacy. She specializes in the management and surgical treatment of knee, shoulder, and...
View all posts






























Reviews
There are no reviews yet.