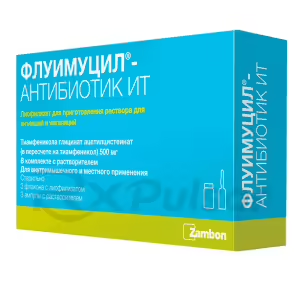
Buy Thiamphenicol Glycinate Acetylcysteinate
Understanding Thiamphenicol Glycinate Acetylcysteinate
Respiratory tract infections are a common ailment, impacting millions worldwide. Effective treatment often requires a multi-pronged approach targeting both the infection and the associated mucus buildup. Thiamphenicol glycinate acetylcysteinate (TGA) represents a novel combination therapy designed to address this dual challenge.
TGA combines the antibacterial power of thiamphenicol with the mucolytic properties of acetylcysteine. This synergistic approach aims for superior efficacy compared to using either component alone. Research suggests this combination may offer advantages in treating certain respiratory infections characterized by excessive mucus.
The unique formulation of TGA is intended to enhance both drug delivery and overall therapeutic outcome. Studies have explored its effectiveness against a range of bacterial pathogens frequently associated with respiratory infections, including Haemophilus influenzae and various streptococcal species. Further research is ongoing to fully elucidate its clinical potential.
Understanding the mechanism of action of TGA involves considering both its antibacterial and mucolytic components. Thiamphenicol, a broad-spectrum antibiotic, works by inhibiting bacterial protein synthesis. Acetylcysteine, a mucolytic agent, helps break down and thin the mucus, aiding in its removal from the respiratory tract.
Clinical trials have demonstrated TGA’s potential benefits in treating acute respiratory infections complicated by mucus buildup. However, it’s crucial to remember that the effectiveness of TGA, like any medication, varies depending on the specific infection and individual patient factors. Always consult with a healthcare professional for appropriate diagnosis and treatment.
A Powerful Combination
Thiamphenicol glycinate acetylcysteinate (TGA) isn’t just a simple blend; it’s a carefully orchestrated duet of therapeutic actions. This isn’t your typical “one-size-fits-all” approach. Instead, TGA combines the strengths of two distinct yet complementary components to create a powerful synergy against respiratory infections.
Think of it like this: you’ve got a stubborn infection (the villain) and thick, obstructive mucus (its accomplice). Thiamphenicol, a broad-spectrum antibiotic, directly combats the bacterial infection, acting as the hero. Simultaneously, acetylcysteine, a potent mucolytic agent, steps in to dismantle the mucus, clearing the battlefield for the antibiotic to work its magic. This dual action is key.
This combined approach addresses the core challenges of many respiratory infections. Many treatments focus solely on killing bacteria, overlooking the crucial role of mucus in hindering treatment efficacy and prolonging recovery. TGA tackles both problems head-on, aiming for faster and more complete resolution of symptoms. Clinical studies have explored this dual-action mechanism, focusing on improved bacterial clearance and reduced mucus viscosity.
The combined effect of TGA isn’t merely additive; it’s synergistic. This means that the combined effect is greater than the sum of its parts, leading to a more potent therapeutic outcome. The improved efficacy could translate into shorter recovery times, reduced symptom severity, and potentially decreased antibiotic resistance development. This makes TGA a potentially valuable option in managing specific types of respiratory infections.
The clever combination in TGA means that it addresses both the infection itself and the physical impediment of thick mucus. This two-pronged approach might offer significant advantages over treatments that only target one aspect of the problem. Further research is needed to fully understand the full therapeutic potential of this innovative combination.
What is Thiamphenicol Glycinate Acetylcysteinate (TGA)?
Imagine a respiratory infection leaving you struggling to breathe, choked by thick, sticky mucus. That’s where Thiamphenicol Glycinate Acetylcysteinate (TGA) comes in. It’s not just one drug, but a powerful combination designed to tackle both the infection and the mucus simultaneously. This unique approach makes it stand out from many traditional treatments.
At its core, TGA is a synergistic blend of two key components: thiamphenicol and acetylcysteine. Thiamphenicol is a broad-spectrum antibiotic, effectively targeting a wide range of bacteria commonly responsible for respiratory infections. This antibiotic component helps directly combat the infection.
Acetylcysteine, on the other hand, plays a crucial mucolytic role. It acts as a mucus thinner, breaking down the thick, tenacious secretions that often clog airways and worsen symptoms. By reducing mucus viscosity, it improves airflow and enhances the effectiveness of the antibiotic. This action addresses the physical barrier to recovery.
The combined effect of these two active ingredients is what makes TGA unique. It isn’t simply the sum of its parts; the synergy between the antibiotic and the mucolytic allows for a more comprehensive and effective treatment strategy. Studies suggest this could lead to faster symptom relief and improved overall patient outcomes compared to single-agent therapies. This is a key difference.
Therefore, TGA is more than just an antibiotic or a mucolytic; it’s a targeted approach to respiratory infections. By simultaneously combating the infection and clearing the airways of obstructing mucus, TGA offers a more holistic strategy for resolving respiratory issues. This dual mechanism is critical for success.
Mechanism of Action
Understanding how Thiamphenicol Glycinate Acetylcysteinate (TGA) works requires looking at the individual actions of its two key components and how they interact synergistically. It’s a two-pronged attack on respiratory infections, targeting both the infection and the physical barrier of mucus.
The antibacterial action comes from thiamphenicol. This broad-spectrum antibiotic works by interfering with bacterial protein synthesis, essentially stopping the bacteria from making the components they need to survive and reproduce. This directly tackles the infectious agent driving the illness.
Meanwhile, the mucolytic effect is provided by acetylcysteine. This molecule breaks down disulfide bonds within the mucus, reducing its viscosity. This thinning action makes it easier to cough up and expel the mucus, clearing the airways and improving lung function. This is crucial for effective breathing and overall recovery.
The true power of TGA lies in the synergy between these two actions. By simultaneously tackling the bacterial infection and reducing the obstructive mucus, TGA aims for a more complete and efficient resolution of the infection. This combined approach potentially leads to faster recovery and reduced symptom duration compared to using either component alone.
In essence, TGA’s mechanism is a clever combination of direct antimicrobial activity and physical airway clearance. This two-pronged approach addresses the multifaceted nature of many respiratory infections, aiming for a more comprehensive and effective treatment strategy. The combined effects are often greater than the sum of the individual parts.
Antibacterial Effects of Thiamphenicol
Thiamphenicol, the antibiotic component of TGA, plays a crucial role in fighting respiratory infections. Its effectiveness stems from its ability to target and inhibit bacterial growth, a key factor in resolving the infection. This direct action is vital for a successful recovery.
Specifically, thiamphenicol works by binding to bacterial ribosomes. These ribosomes are essential for bacterial protein synthesis; by blocking their function, thiamphenicol prevents bacteria from producing the proteins necessary for survival and replication. This mechanism effectively halts bacterial growth and proliferation.
The broad-spectrum nature of thiamphenicol is another key advantage. It’s effective against a wide range of bacterial species, making it a valuable tool in treating infections caused by various pathogens. This wide-ranging activity is particularly helpful when the specific causative bacteria aren’t immediately known. This reduces the need for specific testing.
However, it’s important to note that while thiamphenicol is effective against many bacteria, it’s not a universal cure-all. Antibiotic resistance is an ever-growing concern, and the susceptibility of specific bacterial strains to thiamphenicol can vary. It’s crucial to remember that antibiotics should only be used when necessary, under the guidance of a healthcare professional.
Therefore, while thiamphenicol’s antibacterial action is a cornerstone of TGA’s effectiveness, responsible use and understanding of its limitations are paramount. The precise mechanism and spectrum of activity underscore its importance in combating bacterial respiratory infections. This targeted action is a key element in TGA’s overall strategy.
Mucolytic Action of Acetylcysteine
Acetylcysteine, the mucolytic component of TGA, plays a vital supporting role in treating respiratory infections. Its primary function is to break down and thin the thick, viscous mucus often associated with these infections. This is crucial because excessive mucus can obstruct airways, hindering breathing and reducing the effectiveness of antibiotics.
The mechanism of action involves the disruption of disulfide bonds within the mucus. These bonds are responsible for the mucus’s sticky, gel-like consistency. By breaking these bonds, acetylcysteine reduces the viscosity of the mucus, making it easier to expectorate (cough up) and clear from the respiratory tract. This physical clearance is key.
This mucolytic effect is not merely a convenience; it directly enhances the overall effectiveness of the treatment. By clearing the airways of obstructing mucus, acetylcysteine facilitates better penetration of the antibiotic to the infection site. This improved access allows the thiamphenicol to work more efficiently, leading to better bacterial clearance.
Moreover, improved airway clearance contributes to symptom relief. The reduced mucus buildup leads to easier breathing, less coughing, and a general improvement in respiratory function. These symptomatic improvements significantly enhance patient comfort and quality of life during recovery. This is a significant clinical benefit.
In summary, acetylcysteine’s mucolytic action complements the antibacterial effect of thiamphenicol. This synergistic effect makes TGA a more comprehensive and effective treatment option for respiratory infections characterized by excessive mucus production. This dual action is key to its success.
Clinical Applications
Thiamphenicol glycinate acetylcysteinate (TGA) shows promise in several clinical settings, particularly those involving respiratory infections complicated by excessive mucus production. Its dual mechanism of action makes it a potentially valuable treatment option where both bacterial clearance and mucus reduction are crucial for recovery.
Acute bronchitis, characterized by inflammation of the bronchial tubes and often accompanied by significant mucus buildup, is one area where TGA could be beneficial. The combined action of the antibiotic and mucolytic could lead to faster resolution of symptoms and improved lung function compared to treatments focusing solely on bacterial eradication. This is a key application.
Pneumonia, a more serious lung infection, often presents with mucus accumulation that can impair gas exchange and worsen the disease course. In such cases, TGA’s ability to both combat the infection and clear the airways could offer significant advantages, contributing to improved patient outcomes and reduced hospitalization rates. This demonstrates its potential for broader use.
Other potential applications of TGA might include certain types of sinusitis and bronchiectasis, conditions where mucus buildup is a major contributing factor. However, further research is needed to fully evaluate the efficacy and safety of TGA in these specific contexts. This highlights areas for future research.
It’s important to remember that TGA, like any medication, should be used under the guidance of a healthcare professional. The specific clinical application will always depend on the individual patient’s condition, the causative organism, and other relevant clinical factors. This approach ensures responsible and effective use.
Comparative Efficacy
Evaluating the efficacy of Thiamphenicol Glycinate Acetylcysteinate (TGA) requires comparing it to other treatment options for similar respiratory infections. Direct comparisons are crucial for understanding its potential advantages and disadvantages in clinical practice. This comparative analysis informs treatment choices.
Studies have compared TGA to various antibiotics commonly used for respiratory infections. In some cases, TGA demonstrated comparable efficacy to these agents, while in others, TGA showed superior outcomes, particularly in situations where significant mucus production complicated the infection. This highlights its potential advantage in specific cases.
The inclusion of acetylcysteine in TGA is a key differentiator. Many conventional antibiotic treatments don’t address the issue of mucus buildup, which can hinder drug delivery and prolong recovery. TGA’s mucolytic component potentially offers a significant advantage by improving airway clearance and enhancing the overall therapeutic effect. This is a substantial difference.
However, it’s important to acknowledge limitations in direct comparisons. Study designs, patient populations, and outcome measures can vary significantly across different trials, making it challenging to draw definitive conclusions. Further well-designed, head-to-head studies are needed to solidify the comparative efficacy of TGA. This underscores the need for more research.
Therefore, while preliminary evidence suggests potential advantages of TGA over some conventional treatments, especially in mucus-heavy infections, more rigorous comparative studies are essential to firmly establish its position in clinical guidelines. This emphasizes the ongoing importance of clinical trials.
Pros of TGA
Thiamphenicol glycinate acetylcysteinate (TGA) offers several potential advantages over traditional treatments for respiratory infections, particularly those complicated by excessive mucus. These benefits stem from its unique dual mechanism of action and could significantly improve patient outcomes.
One key advantage is its synergistic effect. The combined action of thiamphenicol (antibiotic) and acetylcysteine (mucolytic) is often greater than the sum of its parts. This leads to more effective bacterial clearance and improved airway clearance, potentially resulting in faster recovery times and reduced symptom severity. This is a significant benefit.
The mucolytic action of acetylcysteine is a major plus. Many antibiotic treatments for respiratory infections don’t address the issue of mucus buildup, which can hinder drug delivery and prolong symptoms. By thinning the mucus, TGA facilitates better antibiotic penetration and improves airflow, leading to more effective treatment. This is a crucial advantage.
TGA may also offer a broader spectrum of activity compared to some single-antibiotic treatments. Its effectiveness against a range of bacterial pathogens could make it a valuable option in situations where the specific causative organism is unknown. This reduces the need for initial diagnostic tests in some cases.
Finally, the potential for reduced antibiotic resistance is an important consideration. By improving the effectiveness of the antibiotic through better airway clearance, TGA might lessen the selective pressure that contributes to the development of antibiotic-resistant bacteria. This is particularly relevant in the current healthcare landscape.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Lewis B Rappaport, MD [Medical reviewer]
Lewis B Rappaport, MD [Medical reviewer]Dr. Lewis Rappaport is a highly experienced and respected cardiologist who serves as a salaried specialist and consultant for the licensed online pharmacy, RxPulsar.com. With over 30 years of practice...
View all posts