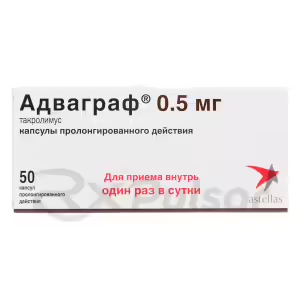
ADVAGRAF™ prolonged-release capsules 0.5mg, 50pcs
$91.00ADVAGRAF™ prolonged-release capsules 1mg, 50pcs
$197.00ADVAGRAF™ prolonged-release capsules 5mg, 50pcs
$1,011.00PROGRAF™ capsules 0.5mg, 50pcs
$87.00PROGRAF™ capsules 1mg, 50pcs
$176.00PROTOPIC™ ointment 0.03%, 30g (1pc)
$68.00TACROLIMUS capsules 0.5mg, 50pcs
$80.00TACROLIMUS capsules 1mg, 50pcs
$154.00TACROPIC™ ointment 0.03%, 15g
$31.00TACROPIC™ ointment 0.1% (15g), 1pc
$35.00Buy Tacrolimus
Tacrolimus: A Powerful Immunosuppressant
Imagine a medication so potent it can prevent your body from rejecting a life-saving organ transplant. That’s the power of tacrolimus, a drug that has revolutionized transplantation medicine and found a niche in dermatology too. Its complex mechanism of action makes it a fascinating and crucial player in the medical world.
Tacrolimus, also known by its brand name Prograf, is a macrolide immunosuppressant. It’s a powerful tool, but like many such potent medicines, it comes with a list of potential side effects that need careful consideration. Understanding its role and impact is critical for both medical professionals and patients.
This article will delve into the intricacies of tacrolimus, exploring its mechanism of action, medical applications, side effects, and overall significance in modern medicine. We’ll attempt to unpack its complex profile in a clear and concise manner.
Tacrolimus, a medication with a significant impact on the field of transplantation and dermatology, stands as a powerful example of how targeted immunosuppression can dramatically improve patient outcomes. Its ability to modulate the immune response has made it invaluable in preventing organ rejection and managing certain inflammatory skin conditions. However, this potent effect also carries potential risks, highlighting the crucial need for careful monitoring and management.
This potent immunosuppressant works by selectively targeting specific components of the immune system, thereby reducing the risk of transplant rejection and inflammation. This targeted approach minimizes the widespread suppression seen with older immunosuppressants. This makes tacrolimus a cornerstone of modern transplant protocols, and also a valuable treatment for recalcitrant skin diseases.
Mechanism of Action: How Tacrolimus Works
Tacrolimus exerts its powerful immunosuppressive effects through a highly specific mechanism, primarily centered around the inhibition of calcineurin. This crucial enzyme plays a pivotal role in the activation of T-cells, the key players in the body’s cellular immune response. By binding to a protein called FKBP-12, tacrolimus forms a complex that effectively blocks calcineurin’s activity.
This blockage of calcineurin has cascading effects on the immune system. It prevents the transcription of genes essential for the production of interleukin-2 (IL-2), a cytokine that promotes T-cell proliferation and activation. The resulting decrease in IL-2 production significantly dampens the immune response, preventing the rejection of transplanted organs and reducing inflammation in conditions like atopic dermatitis.
In simpler terms, tacrolimus acts like a carefully calibrated brake on the immune system’s gas pedal. It doesn’t shut down the immune system entirely, which would leave the body vulnerable to infections, but rather selectively reduces its hyperactivity in specific situations, allowing for controlled immune modulation without crippling the body’s defenses. This targeted approach is key to tacrolimus’s therapeutic efficacy.
Calcineurin Inhibition
At the heart of tacrolimus’s mechanism lies its potent inhibition of calcineurin, a crucial phosphatase enzyme. This enzyme plays a vital role in the intricate signaling pathways that govern T-cell activation. Think of calcineurin as a key conductor of the immune orchestra; tacrolimus silences this conductor, thus dampening the overall immune response.
The inhibition process begins when tacrolimus binds to the immunophilin FKBP12. This binding creates a complex that specifically targets calcineurin. This complex then physically blocks calcineurin’s ability to dephosphorylate other proteins involved in T-cell activation, essentially preventing a critical step in the activation cascade.
The result of this precise molecular interaction is a significant reduction in T-cell activation and proliferation. This targeted suppression is what makes tacrolimus so effective in preventing organ rejection and managing inflammatory skin conditions while minimizing the broader immunosuppression associated with other drugs. It’s a delicate balance, finely tuned at the molecular level.
Impact on T-Cell Activation
The inhibition of calcineurin by tacrolimus doesn’t just stop at the enzyme level; it has profound downstream effects on T-cell activation, the linchpin of the adaptive immune response. This is where the clinical significance of tacrolimus truly shines, preventing the body’s immune system from attacking transplanted organs or causing excessive inflammation in the skin.
Specifically, the blockade of calcineurin prevents the dephosphorylation and subsequent activation of nuclear factor of activated T-cells (NFAT). NFAT is a crucial transcription factor that regulates the expression of numerous genes involved in T-cell proliferation and cytokine production, including the vital interleukin-2 (IL-2).
With NFAT’s activity curtailed, the production of IL-2 and other pro-inflammatory cytokines is significantly reduced. This dampening of the immune response is precisely what makes tacrolimus so effective in preventing organ rejection and managing inflammatory skin diseases like atopic dermatitis. The cascade of events, starting with calcineurin inhibition, ultimately leads to a more controlled and less aggressive immune response.
Medical Applications: Where Tacrolimus Shines
Tacrolimus’s potent immunosuppressive properties have carved a significant niche for itself in various medical fields. Its primary application, and the one that catapulted it to prominence, is in organ transplantation. Here, it acts as a crucial bulwark against the body’s natural tendency to reject foreign tissue, significantly improving the success rates of transplants.
Beyond transplantation, tacrolimus has found a valuable role in dermatology, specifically in the management of atopic dermatitis (eczema). In this context, its topical application helps to control the inflammation and itching associated with this chronic skin condition, offering relief to many sufferers. This application showcases the drug’s versatility and targeted action.
The success of tacrolimus in these areas stems from its ability to finely tune the immune response. It doesn’t completely shut down the immune system, leaving patients vulnerable to infections, but rather selectively dampens the overactive immune responses that cause organ rejection and eczema flare-ups. This targeted approach underscores the precision of its mechanism and its value in treating complex immune-mediated conditions.
Organ Transplantation
In the realm of organ transplantation, tacrolimus stands as a cornerstone of immunosuppressive therapy. Its ability to prevent the body from rejecting a transplanted organ is nothing short of remarkable, significantly increasing the chances of a successful transplant and long-term survival for recipients. This has revolutionized the field, offering hope to countless individuals.
The drug’s precise mechanism of action, targeting T-cell activation, makes it particularly effective in minimizing the risk of rejection. By selectively dampening the immune response, tacrolimus allows the transplanted organ to integrate into the recipient’s body without triggering a powerful immune attack. This targeted approach minimizes the side effects associated with broader immunosuppression.
Tacrolimus is often used in combination with other immunosuppressants, creating a powerful regimen to maximize the chances of transplant success. However, its use requires careful monitoring of blood levels and potential side effects, emphasizing the need for close collaboration between the transplant team and the patient. The goal is to strike a delicate balance: sufficient immunosuppression to prevent rejection, but not so much as to compromise the patient’s overall health.
Atopic Dermatitis Treatment
Beyond its crucial role in transplantation, tacrolimus has emerged as a valuable treatment option for atopic dermatitis (AD), also known as eczema. This chronic inflammatory skin condition affects millions, causing intense itching, dryness, and skin lesions. Tacrolimus offers a targeted approach to managing these symptoms, particularly in cases where traditional treatments haven’t provided sufficient relief.
Applied topically, tacrolimus effectively reduces inflammation by modulating the immune response within the skin. It selectively targets the overactive immune cells contributing to the characteristic inflammation and itching of AD, without the systemic effects associated with oral immunosuppressants. This localized action minimizes the risk of broader side effects.
The use of tacrolimus in AD is particularly beneficial for its ability to manage inflammation without the side effects often associated with topical corticosteroids, such as skin thinning. While not a cure, it provides significant relief for many patients, improving their quality of life by reducing the debilitating symptoms of this challenging skin condition. It’s often used when other treatments have proven inadequate.
Side Effects: Weighing the Risks
While tacrolimus offers significant therapeutic benefits, it’s crucial to acknowledge the potential side effects. These can range from relatively mild to severe, underscoring the need for careful monitoring and management by healthcare professionals. Understanding these potential risks is key to making informed decisions about treatment.
Common side effects can include headache, nausea, tremor, and increased blood pressure. These are often manageable and may subside as the body adjusts to the medication. However, more serious side effects, though less frequent, require immediate medical attention. These can include kidney problems (nephrotoxicity), increased risk of infection, and neurological issues.
The severity of side effects can vary depending on factors such as dosage, duration of treatment, and individual patient factors. Regular monitoring of blood levels and kidney function is essential, especially in patients receiving systemic tacrolimus. Open communication between patient and physician is key to addressing any concerns and ensuring safe and effective treatment.
Common Side Effects
While the benefits of tacrolimus are significant, it’s important to be aware of the commonly reported side effects. These are usually mild and manageable, often resolving as the body adjusts to the medication. However, it’s crucial to report any side effects to your doctor, as they can help determine the best course of action.
Some of the most frequently reported side effects include headache, nausea, tremor, and increased blood pressure. These can range in severity from barely noticeable to mildly disruptive, depending on the individual. Simple lifestyle adjustments, like staying hydrated or managing stress, can sometimes mitigate these effects.
Other common side effects can include diarrhea, hyperglycemia (high blood sugar), and hyperkalemia (high potassium levels). Your doctor will likely monitor these levels through regular blood tests, allowing for adjustments to the medication or supportive treatments as needed. Understanding these common effects empowers patients to work proactively with their healthcare providers.
Serious Side Effects
While less common than the milder side effects, the potential for serious adverse reactions with tacrolimus necessitates careful monitoring and prompt medical attention if they occur. These serious side effects, though infrequent, can significantly impact a patient’s health and require immediate intervention. Open communication with your doctor is paramount.
One of the most concerning serious side effects is kidney damage (nephrotoxicity). This can manifest as decreased urine output, swelling in the legs and ankles, or changes in blood test results indicating kidney dysfunction. Regular monitoring of kidney function through blood tests is crucial to detect and manage this potential complication.
Other serious side effects include increased susceptibility to infections due to immunosuppression, neurological problems such as seizures or tremors, and liver dysfunction. These conditions require immediate medical attention and may necessitate adjustments to the medication or additional supportive therapies. Early detection and intervention are key to minimizing potential long-term consequences.
Tacrolimus – A Double-Edged Sword
Pros of Tacrolimus
Tacrolimus offers several significant advantages in its therapeutic applications. Its effectiveness in preventing organ rejection in transplantation is a major benefit, offering patients a greatly increased chance of a successful transplant and a better quality of life. This life-saving potential is a testament to the drug’s power.
In the treatment of atopic dermatitis, tacrolimus provides a valuable alternative to topical corticosteroids, reducing inflammation and itching without the side effects of long-term steroid use, such as skin thinning. This targeted approach makes it an attractive option for patients with chronic eczema.
Furthermore, tacrolimus’s mechanism of action, focusing on specific aspects of the immune response, allows for a more targeted approach to immunosuppression compared to older, broader-acting medications. This targeted action minimizes the risk of widespread immunosuppression, which can lead to increased vulnerability to infections. This precision is a key advantage.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Lewis B Rappaport, MD [Medical reviewer]
Lewis B Rappaport, MD [Medical reviewer]Dr. Lewis Rappaport is a highly experienced and respected cardiologist who serves as a salaried specialist and consultant for the licensed online pharmacy, RxPulsar.com. With over 30 years of practice...
View all posts