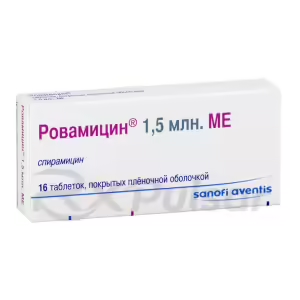
Buy Spiramycin
Understanding Spiramycin: A Macrolide Antibiotic
Spiramycin, a fascinating member of the macrolide antibiotic family, holds a unique place in the world of medicine. Its history stretches back to 1954, when it was first isolated, showcasing its long-standing role in combating infections.
Unlike some antibiotics with broad-spectrum activity, spiramycin demonstrates selective targeting. This characteristic makes it particularly valuable in specific situations where a less disruptive approach is preferred. Its mechanism of action involves inhibiting protein synthesis within susceptible bacteria, effectively halting their growth and reproduction.
This targeted action is a key aspect of its profile. The selective nature of spiramycin minimizes the disruption of the body’s natural bacterial flora, potentially reducing the incidence of common side effects associated with broader-spectrum antibiotics. This is a significant advantage in certain patient populations.
The unique properties of spiramycin have led to its use in diverse clinical settings. Research continues to explore its potential applications and refine our understanding of its role in combating a range of infections. Further investigation into its mechanisms and applications promises exciting developments in the future.
What is Spiramycin?
Spiramycin, a macrolide antibiotic, isn’t your typical antibiotic; it’s a bit of a specialist. Unlike some broad-spectrum antibiotics that tackle a wide range of bacterial infections, spiramycin exhibits a more targeted approach. This specificity is key to its unique applications in medicine.
Derived from the Streptomyces ambofaciens bacterium, spiramycin boasts a distinctive chemical structure – a 16-membered ring macrolide. This structure is crucial to its function; it allows spiramycin to bind to the 50S ribosomal subunit of susceptible bacteria. This binding action effectively disrupts the bacteria’s protein synthesis, a vital process for their survival and replication.
The impact of this disruption is significant. By interfering with protein synthesis, spiramycin prevents the bacteria from producing essential proteins, effectively halting their growth and reproduction. This mechanism is the foundation of spiramycin’s effectiveness against specific bacterial and even parasitic infections.
Its unique mechanism and targeted action set it apart. This focused approach minimizes the disruption to the body’s beneficial bacterial flora, which can be a significant advantage, especially when compared to the broader effects of other antibiotics. This selective action is what makes spiramycin such a valuable tool in the physician’s arsenal.
Interestingly, spiramycin’s high concentration in tonsillar lymphoid tissue has prompted research into its potential preventive role against certain infections. However, it’s important to note that it doesn’t reach the cerebrospinal fluid, limiting its application in treating infections affecting this area of the body. Further research continues to explore the full potential of this fascinating antibiotic.
Uses of Spiramycin
Spiramycin’s therapeutic applications are noteworthy for their specificity. While not a broad-spectrum antibiotic, its unique properties make it a valuable tool in certain clinical situations. Its targeted action minimizes disruption to the body’s beneficial bacteria, a significant advantage.
One of its primary uses is in the management of toxoplasmosis, particularly in pregnant women. This parasitic infection can be particularly dangerous for the developing fetus, and spiramycin plays a crucial role in mitigating the risk of transmission from mother to child. The drug’s ability to reduce the risk of congenital toxoplasmosis is a cornerstone of its clinical use.
Beyond its use in combating toxoplasmosis, spiramycin has shown efficacy against certain bacterial infections. It’s often used to treat infections caused by susceptible Gram-positive bacteria, although it’s not a first-line treatment for most bacterial infections. The physician will carefully consider the specific infection and the patient’s individual circumstances when determining if spiramycin is appropriate.
Another area where spiramycin might be considered is in patients allergic to penicillin. In cases of gonorrhea, for example, where penicillin is typically the treatment of choice, spiramycin can offer a viable alternative for patients with penicillin allergies. This highlights its role in addressing specific sensitivities and allergies.
Finally, ongoing research continues to explore potential uses of spiramycin. Its unique properties and selective nature suggest that further investigations might reveal additional therapeutic applications, expanding its role in the future of infectious disease management. The focus remains on refining its use in targeted scenarios where its specific benefits shine.
Dosage and Administration
Determining the appropriate dosage and administration of spiramycin is crucial for effective treatment and minimizing potential side effects. Dosage regimens are highly individualized, tailored to the specific infection being treated, the patient’s overall health, and other relevant factors. It’s essential to follow a physician’s precise instructions.
The form of spiramycin (e.g., tablets, suspension) will influence administration. Oral administration is common for many applications, often involving a specific dosage schedule. For instance, a physician might prescribe a particular number of tablets or milliliters of suspension to be taken at set intervals throughout the day. Strict adherence to this schedule is vital.
The duration of treatment is another critical consideration. The length of treatment will vary depending on the type and severity of the infection. A physician will determine the appropriate treatment duration based on factors such as the patient’s response to treatment and the overall course of the infection. Premature discontinuation of treatment can lead to treatment failure.
In some cases, particularly with severe or complex infections, a physician might adjust the dosage or administration route. Such adjustments might be made in response to the patient’s response to treatment, the emergence of resistance, or other relevant clinical factors. Close monitoring of the patient’s condition is therefore necessary.
Remember: This information is for general understanding only. Never attempt to self-medicate or alter your prescribed dosage without consulting your physician. Your doctor will determine the optimal dosage, administration method, and duration of treatment based on your unique circumstances.
Side Effects of Spiramycin
While generally well-tolerated, spiramycin, like any medication, can produce side effects. It’s crucial to remember that not everyone experiences these, and the severity can vary greatly from person to person. Understanding the potential side effects allows for proactive management and prompt medical attention if needed.
Gastrointestinal issues are among the most commonly reported side effects. These can range from mild discomfort, such as nausea, vomiting, or diarrhea, to more severe problems. Less frequently, individuals might experience abdominal pain or indigestion. If you experience any of these symptoms, it’s advisable to contact your healthcare provider.
Allergic reactions, though less common, are a possibility. These reactions can manifest in various ways, from mild skin rashes and itching to more severe symptoms like angioedema (swelling of the deeper layers of skin) or anaphylactic shock. In the event of an allergic reaction, immediate medical attention is crucial. Early intervention can be vital.
In rarer instances, more serious side effects have been reported. These include hepatic issues such as cholestatic hepatitis, as well as hematological effects like hemolytic anemia. These are less frequent occurrences, but their potential severity necessitates prompt medical evaluation should they arise. Your physician will carefully assess your risk factors.
It’s important to note that this list isn’t exhaustive. Other, less frequently observed side effects are possible. Always inform your doctor about any new or unusual symptoms you experience while taking spiramycin. Open communication with your physician is key to safe and effective treatment.
Pros of Spiramycin
Spiramycin offers several advantages, making it a valuable therapeutic option in specific clinical situations. Its unique profile sets it apart from broader-spectrum antibiotics, offering benefits that are particularly relevant in certain patient populations.
One key advantage is its targeted action. Unlike many antibiotics that disrupt the body’s natural bacterial balance, spiramycin’s more selective nature minimizes this disruption. This can translate to a reduced risk of side effects associated with broad-spectrum antibiotic use, such as gut dysbiosis.
Its effectiveness against toxoplasmosis, especially in pregnant women, is another significant pro. This targeted efficacy helps protect both the mother and the developing fetus from the potentially serious consequences of this parasitic infection. This is a crucial advantage in a vulnerable population.
Spiramycin’s role as an alternative for patients with penicillin allergies is also a major benefit. For those with penicillin allergies, spiramycin can provide a safe and effective treatment option in cases where penicillin would typically be the drug of choice. This expands treatment options for a significant patient group.
Finally, the generally favorable tolerability profile of spiramycin is a notable advantage. While side effects are possible, they are often mild and less frequent compared to some broader-spectrum antibiotics. This makes it a potentially better-tolerated option for patients who might be sensitive to other medications.
Cons of Spiramycin
While spiramycin offers significant advantages, it’s important to acknowledge potential drawbacks. Understanding these limitations helps ensure appropriate and safe use of the medication. These potential downsides are important considerations for both physicians and patients.
One significant limitation is spiramycin’s narrow spectrum of activity. Unlike broad-spectrum antibiotics, its effectiveness is confined to a specific range of bacteria and parasites. This means it won’t be effective against a wide array of infections, limiting its applicability in many situations.
The potential for side effects, although often mild, should not be overlooked. Gastrointestinal upset, including nausea, vomiting, and diarrhea, are relatively common. While generally manageable, these side effects can impact a patient’s quality of life and adherence to treatment. Careful monitoring is crucial.
Another consideration is the possibility of allergic reactions. While infrequent, allergic reactions to spiramycin can range from mild skin rashes to severe anaphylaxis. This underscores the need for careful monitoring and prompt medical attention if any allergic symptoms develop. Early intervention is key.
Finally, the emergence of antibiotic resistance is an ongoing concern for all antibiotics, including spiramycin. Overuse or inappropriate use of antibiotics contributes to the development of resistant strains, making treatment more challenging. Judicious use guided by proper medical diagnosis is paramount.
Considerations for Specific Patient Groups
When prescribing spiramycin, healthcare professionals must consider the unique needs and potential vulnerabilities of specific patient populations. Careful assessment and individualized treatment plans are crucial for optimal outcomes and minimized risks. This tailored approach is essential for patient safety.
For instance, pregnant women represent a unique group. While spiramycin is often used to treat toxoplasmosis during pregnancy, the potential impact on fetal development necessitates careful monitoring and a thorough risk-benefit analysis. The decision to use spiramycin during pregnancy is made on a case-by-case basis, considering the severity of the infection and potential risks.
Similarly, older adults may require dosage adjustments due to potential age-related changes in liver and kidney function. These changes can affect the metabolism and excretion of spiramycin, potentially leading to increased risk of side effects or reduced efficacy if standard dosages are used. Dosage adjustments are often necessary.
Patients with pre-existing liver or kidney disease also warrant special attention. Since spiramycin is primarily metabolized by the liver and excreted by the kidneys, impairment of these organs can lead to drug accumulation and increased risk of adverse events. Close monitoring of liver and kidney function is essential during treatment.
Finally, the potential interactions with other medications must be considered. Concurrent use of spiramycin with certain drugs might necessitate dosage adjustments or alternative treatment options. A comprehensive review of the patient’s medication history is crucial to avoid harmful interactions. Your doctor will consider all your medications.
Pregnancy and Breastfeeding:
The use of spiramycin during pregnancy and breastfeeding requires careful consideration due to the potential impact on both the mother and the developing child. Decisions regarding spiramycin use during these periods should always be made in consultation with a healthcare professional who can weigh the potential benefits against the risks.
In pregnancy, spiramycin is sometimes used to treat toxoplasmosis, a parasitic infection that can pose significant risks to the developing fetus. However, the decision to use spiramycin during pregnancy is made on a case-by-case basis, carefully weighing the potential benefits of treating the infection against the potential risks to the fetus. This is a complex decision.
During breastfeeding, spiramycin is known to be excreted in breast milk. While the amounts typically present in breast milk are generally considered low, the potential impact on the nursing infant should be carefully evaluated. The physician will consider the infant’s age, health, and the mother’s clinical condition when making recommendations.
The potential risks associated with spiramycin use during pregnancy and breastfeeding necessitate close monitoring of both the mother and the child. Regular check-ups and careful assessment of the infant’s health are crucial to ensure early detection and management of any potential adverse effects. This proactive approach is essential.
Ultimately, the decision of whether or not to use spiramycin during pregnancy or breastfeeding is highly individualized and depends on several factors. A thorough discussion with a healthcare provider is essential to ensure the safest and most effective approach for both the mother and the child. This personalized approach is key.
Older Adults:
Older adults often require special considerations when prescribed medications, and spiramycin is no exception. Age-related physiological changes can influence how the body processes drugs, potentially impacting both efficacy and safety. Therefore, a tailored approach is crucial for this population.
One key consideration is the potential for reduced renal and hepatic function in older adults. These organs play vital roles in drug metabolism and excretion. Impaired function can lead to increased drug accumulation, raising the risk of adverse effects. Careful monitoring is therefore essential.
Another factor to consider is the increased prevalence of comorbidities in older adults. The presence of other medical conditions, such as heart disease or liver problems, can interact with spiramycin, potentially increasing the risk of adverse events. A thorough medical history is vital.
Dosage adjustments may be necessary to account for age-related physiological changes. Lower dosages or less frequent administration might be considered to reduce the risk of adverse events while still achieving therapeutic effects. This personalized approach is paramount.
Finally, close monitoring for side effects is particularly important in older adults. They may be more sensitive to the effects of medications and may experience adverse events more severely. Regular check-ups and prompt attention to any new or worsening symptoms are crucial. Proactive care is essential.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Jessica Kerns, MD [Medical reviewer]
Jessica Kerns, MD [Medical reviewer]Dr. Jessica Kerns is a highly accomplished pediatrician and adolescent medicine specialist who serves as a clinical instructor in the Department of Pediatrics at the Icahn School of Medicine at Mount...
View all posts