Buy Glatiramer Acetate
Understanding Glatiramer Acetate
Multiple sclerosis (MS) is a challenging neurological condition, and finding effective treatments is crucial for improving patients’ lives. Glatiramer acetate (GA) has emerged as a significant player in MS management, offering a unique approach to disease modification.
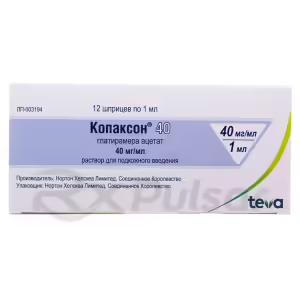
Glatiramer acetate, also known by the brand name Copaxone, is a synthetically produced polypeptide. It’s a complex mixture of amino acids, designed to mimic components of myelin, the protective sheath around nerve fibers.
The exact mechanism of action isn’t fully understood, but research suggests GA modulates the immune system. This modulation helps to reduce the frequency and severity of MS relapses.
GA’s impact on the immune system involves several key processes. It influences the activity of different types of immune cells, shifting the balance towards an anti-inflammatory state.
A Novel Approach to Multiple Sclerosis Treatment
Multiple sclerosis (MS) disrupts the communication pathways of the brain and spinal cord, leading to a range of debilitating symptoms. Traditional treatments often focused on managing symptoms, but glatiramer acetate offers a different approach: disease modification. Instead of merely treating symptoms, it aims to alter the underlying disease process.
Unlike some MS therapies that suppress the entire immune system, glatiramer acetate works by selectively modulating the immune response. This targeted approach minimizes the risk of broad immunosuppression, a common side effect of other treatments that can leave patients vulnerable to infections.
The way glatiramer acetate achieves this modulation is fascinating and still under investigation. It appears to influence the balance between different types of immune cells, shifting the response away from inflammation and towards a more protective state. This nuanced interaction with the immune system is what sets glatiramer acetate apart.
This targeted immune modulation is a significant advancement in MS treatment. By focusing on specific immune pathways implicated in MS, glatiramer acetate strives to reduce the damage to the myelin sheath and slow disease progression, ultimately improving long-term outcomes for patients. It represents a more refined strategy compared to broad immunosuppression.
Mechanism of Action: Unraveling the Mystery
While the precise way glatiramer acetate works remains an area of ongoing research, scientists have pieced together a complex picture involving several key interactions within the immune system. It’s not a simple “on/off” switch but a sophisticated dance of cellular communication.
One crucial aspect appears to be the modulation of T-cell activity. These cells, key players in the immune response, are implicated in the autoimmune attack on myelin in MS. Glatiramer acetate seems to influence the balance between different types of T-cells, shifting the response towards a less damaging profile.
Antigen-presenting cells (APCs) play a critical role in this process. These cells present antigens (foreign substances) to T-cells, initiating an immune response. Glatiramer acetate interacts with APCs, potentially altering the way they present antigens and thereby influencing the subsequent T-cell response. This interaction is subtle but impactful.
The production of cytokines, signaling molecules that mediate communication between immune cells, is also affected. Glatiramer acetate appears to influence the types of cytokines produced, shifting the balance from pro-inflammatory (damaging) cytokines to anti-inflammatory (protective) ones. This shift is crucial in dampening the autoimmune attack.
In summary, the mechanism of glatiramer acetate involves a complex interplay between T-cells, APCs, and cytokines. The result is a shift towards an anti-inflammatory state, reducing the damaging immune response characteristic of MS. Further research will undoubtedly provide a more detailed understanding of this intricate process.
Immune System Modulation
Understanding how glatiramer acetate impacts the immune system is key to appreciating its therapeutic effects in multiple sclerosis. It’s not a simple suppression of the entire immune response, but rather a carefully orchestrated shift in its activity. Think of it as fine-tuning an orchestra rather than silencing it completely.
The drug’s primary mechanism involves influencing the balance between different types of immune cells. In MS, the immune system mistakenly attacks the myelin sheath, causing inflammation and nerve damage. Glatiramer acetate appears to redirect this response, promoting a less aggressive, more protective state.
This modulation isn’t a one-size-fits-all approach. Instead, it involves several interacting pathways. It influences the activity of T-cells, key players in the immune response, and interacts with antigen-presenting cells (APCs), which initiate immune reactions. The net effect is a reduction in the damaging immune response directed at the myelin.
Furthermore, the production of cytokines, signaling molecules that regulate immune cell activity, is also altered. Glatiramer acetate appears to favor the production of anti-inflammatory cytokines while reducing the levels of pro-inflammatory cytokines. This carefully orchestrated shift in cytokine profiles helps to reduce the overall inflammatory response in the central nervous system.
In essence, glatiramer acetate’s impact on the immune system is multifaceted and subtle, yet highly effective in modifying the disease course of MS. This intricate modulation is what differentiates it from other, more broadly suppressive immunotherapies.
Key Players: T-Cells and Cytokines
The immune system’s response in multiple sclerosis (MS) is complex, involving a cast of characters that work togetherâor, in this case, sometimes against each other. Glatiramer acetate’s mechanism of action cleverly targets several key players in this intricate dance.
T-cells are central to the autoimmune attack in MS. These immune cells, normally tasked with defending against infections, mistakenly target the myelin sheath surrounding nerve fibers. Glatiramer acetate doesn’t simply suppress all T-cells; instead, it appears to modulate their activity, influencing the balance between different T-cell subsets.
This modulation involves a shift towards a less damaging profile. The drug seems to promote the expansion of regulatory T-cells (Tregs), which help to suppress the autoimmune response. Conversely, it may reduce the number or activity of pro-inflammatory T-cells that contribute to the damage in MS.
Cytokines act as messengers between immune cells, coordinating their activities. Some cytokines promote inflammation, while others dampen it. Glatiramer acetate influences this cytokine network, shifting the balance towards anti-inflammatory cytokines. This change helps to reduce the overall inflammation and tissue damage characteristic of MS.
This targeted approach, focusing on specific T-cell subsets and cytokine profiles, is what makes glatiramer acetate’s mechanism of action so unique and effective. It’s a sophisticated intervention, not a blunt instrument, and its precision is crucial to its therapeutic effects.
Antigen-Presenting Cells (APCs)
Antigen-presenting cells (APCs) are unsung heroes of the immune system, acting as the crucial link between the body’s defenses and invading substances. In multiple sclerosis (MS), their role becomes particularly significant, and glatiramer acetate cleverly exploits this connection.
APCs, such as dendritic cells and macrophages, are responsible for capturing and presenting antigens to T-cells. In MS, they can mistakenly present myelin proteins as foreign invaders, triggering an autoimmune response. Glatiramer acetate appears to interfere with this process, altering the way APCs present antigens.
This interference isn’t about blocking antigen presentation altogether; it’s about subtly changing the message. By interacting with APCs, glatiramer acetate may modify the way they present myelin proteins, reducing the likelihood of triggering a damaging T-cell response. It’s a nuanced intervention, not a shutdown.
Furthermore, the interaction with APCs might lead to a shift in their functional profile. Glatiramer acetate may promote the development of anti-inflammatory APCs, which in turn influence the T-cells they interact with, promoting a less aggressive immune response. This indirect effect on T-cells is a significant part of the drug’s mechanism.
In short, APCs are not simply bystanders in glatiramer acetate’s mechanism of action; they are active participants. By influencing their function, the drug effectively modifies the immune response at its very source, reducing the autoimmune attack on myelin.
Glatiramer Acetate: A Closer Look
Glatiramer acetate’s unique composition and its effects on multiple sclerosis warrant a closer examination. Understanding its structure and therapeutic benefits provides a clearer picture of its role in managing this challenging disease.
The drug is a synthetic polypeptide, a chain of amino acids designed to resemble components of myelin. This structural similarity plays a crucial role in its mechanism of action, influencing the immune system’s response to myelin.
Beyond its structure, its therapeutic effects are multifaceted. Glatiramer acetate’s primary benefit lies in its ability to reduce the frequency and severity of MS relapses, improving patients’ quality of life.
Composition and Structure
Glatiramer acetate’s unique composition is a key factor in its effectiveness. It’s not a single molecule but a complex mixture of synthetic polypeptides, each a chain of amino acids. This complexity contributes to its multifaceted interaction with the immune system.
The main building blocks are four amino acids: L-glutamic acid, L-lysine, L-alanine, and L-tyrosine. These amino acids are arranged in a random sequence, creating a diverse population of polypeptide chains. This randomness is not accidental; it contributes to the drug’s ability to interact with various components of the immune system.
The average length of these polypeptide chains is around 45 amino acids, but the exact composition varies. This variability is crucial; it’s thought to contribute to the drug’s broad-spectrum effects on the immune system, impacting multiple immune cell types and signaling pathways. The resulting heterogeneity is a key feature of glatiramer acetate’s design.
This carefully crafted heterogeneity isn’t just a random assortment. It’s a deliberate strategy to create a molecule that can interact with a wide range of immune system components. This complexity is reflected in its multifaceted mechanism of action, influencing both T-cells and antigen-presenting cells, and modulating the production of various cytokines.
The precise structure-activity relationships of glatiramer acetate are still being investigated. However, the current understanding highlights the importance of its complex composition in its therapeutic effectiveness for multiple sclerosis. Ongoing research continues to shed light on the precise roles of individual amino acids and the overall polypeptide heterogeneity in mediating its therapeutic effects.
Therapeutic Effects
Glatiramer acetate’s primary therapeutic benefit lies in its ability to modify the course of multiple sclerosis (MS). This isn’t about a cure, but about significantly impacting the disease’s progression and improving patients’ lives. It’s about managing the unpredictable nature of MS and gaining a sense of control.
Clinical trials have consistently demonstrated glatiramer acetate’s effectiveness in reducing the frequency and severity of MS relapses. These relapses, characterized by periods of worsening symptoms, can be debilitating. By reducing their occurrence, glatiramer acetate helps patients maintain a better quality of life and reduce the impact on their daily routines.
Beyond relapse reduction, there’s evidence suggesting glatiramer acetate may also slow the progression of disability in MS. This is a crucial aspect of MS management, as the disease can lead to progressive neurological impairment. Slowing this progression can greatly improve long-term outcomes for patients, maintaining their independence and mobility.
The exact mechanisms underlying these therapeutic effects are still being investigated, but the impact on the immune system is considered central. By modulating the immune response and reducing inflammation in the central nervous system, glatiramer acetate helps to protect the myelin sheath and reduce nerve damage. This protective effect translates into fewer relapses and slower disease progression.
While glatiramer acetate doesn’t offer a cure for MS, its ability to significantly reduce relapses and slow disability progression makes it a valuable tool in managing this complex and unpredictable disease. It provides patients with a chance to live fuller, more active lives, despite the challenges of MS. The long-term benefits are substantial, offering hope and improved quality of life for many.
Pros and Cons of Glatiramer Acetate
As with any medication, glatiramer acetate presents both advantages and disadvantages. A balanced understanding of these aspects is crucial for informed decision-making in the context of multiple sclerosis treatment.
Weighing the potential benefits against potential drawbacks is key to a personalized approach. Patient-specific factors should always be considered when discussing treatment options.
Pros
Glatiramer acetate offers several significant advantages in the management of multiple sclerosis. Its ability to reduce the frequency and severity of relapses is a major plus, improving patients’ quality of life and reducing the unpredictable nature of the disease. This predictability offers a sense of control, which can be incredibly valuable for those living with MS.
Evidence suggests that glatiramer acetate may also help slow the progression of disability, a crucial aspect of long-term management. This means patients may be able to maintain their independence and mobility for longer, preserving their ability to perform daily tasks and participate in activities they enjoy. The preservation of functional abilities is a substantial benefit.
Compared to some other disease-modifying therapies (DMTs), glatiramer acetate is generally considered well-tolerated. While side effects can occur, they are often mild and manageable. This favorable safety profile makes it an attractive option for many patients who may be hesitant about the potential side effects of more aggressive DMTs. The manageable side effect profile contributes to better treatment adherence.
Furthermore, glatiramer acetate has a long track record of use in MS treatment, providing a wealth of clinical data supporting its efficacy and safety. This extensive experience gives clinicians and patients confidence in its effectiveness. This established history offers reassurance and a strong foundation for its continued use.
Finally, the availability of both brand-name and generic versions of glatiramer acetate enhances accessibility for patients. This increased accessibility can be a crucial factor, ensuring that more individuals can benefit from this valuable treatment option. Increased availability contributes to wider access to effective MS management.
Cons
While glatiramer acetate offers significant benefits, it’s essential to acknowledge potential drawbacks. Although generally well-tolerated, some patients experience injection site reactions, such as redness, swelling, or pain. These reactions are usually mild and temporary, but they can be uncomfortable and may affect treatment adherence. Managing these reactions is crucial for maintaining consistent treatment.
Another potential side effect is the development of lipoatrophy at the injection site. This involves a loss of subcutaneous fat, resulting in a noticeable depression in the skin. While not always severe, it can be cosmetically concerning for some patients. Careful rotation of injection sites is recommended to mitigate this risk. Minimizing this side effect is important for patient satisfaction.
Some patients report flu-like symptoms, such as fever, chills, or muscle aches, particularly after the initial doses. These symptoms typically subside as the body adjusts to the medication. However, they can be distressing, and patients should be informed about this potential side effect. Managing these initial symptoms improves patient comfort and increases treatment compliance.
Furthermore, although glatiramer acetate is generally considered safe, rare but serious allergic reactions have been reported. Patients should be aware of the signs and symptoms of allergic reactions and seek immediate medical attention if they occur. Prompt medical attention is crucial in addressing any severe allergic reactions.
Finally, the need for daily subcutaneous injections can be inconvenient for some patients. This can impact adherence, and patients may need support and strategies to maintain a consistent treatment regimen. Supporting patient adherence is crucial for optimizing treatment outcomes.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Elizabeth Dennis, MD [Medical reviewer]
Elizabeth Dennis, MD [Medical reviewer]Dr. Elizabeth Dennis is a highly skilled Orthopedic Surgeon and consultant for RxPulsar.com, a licensed online pharmacy. She specializes in the management and surgical treatment of knee, shoulder, and...
View all posts