Buy Durvalumab
Durvalumab: A Deep Dive into this Immunotherapy Agent
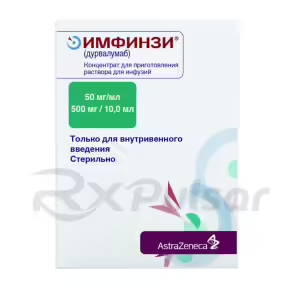
Immunotherapy is revolutionizing cancer treatment, and Durvalumab (Imfinzi) stands as a prominent example. This targeted therapy harnesses the power of the body’s own immune system to fight cancer cells, offering a new approach with potential benefits for various cancers.
Durvalumab’s mechanism of action centers around blocking PD-L1, a protein that helps cancer cells evade detection by the immune system. By inhibiting PD-L1, Durvalumab frees the immune system to recognize and attack cancerous cells more effectively. This innovative approach has shown promising results in several clinical trials, leading to its approval for specific cancer types.
The drug’s development involved extensive research and numerous clinical trials. These trials rigorously assessed Durvalumab’s efficacy and safety profile across different cancer types and stages. The results, published in peer-reviewed journals, have contributed significantly to our understanding of its clinical applications.
Understanding Durvalumab’s role in cancer treatment requires considering both its potential benefits and risks. It’s crucial to discuss the treatment options with your doctor to determine whether it is suitable for your specific circumstances.
Durvalumab, marketed as Imfinzi, represents a significant advancement in cancer immunotherapy. Unlike traditional chemotherapy, which targets rapidly dividing cells, Durvalumab works by specifically targeting and modulating the body’s immune response to cancer. This precision approach aims to minimize harm to healthy cells while maximizing the destruction of cancerous cells. Its mechanism of action, described in detail later, centers on a specific interaction with immune checkpoint proteins.
The development of Durvalumab has been a long and complex process involving extensive preclinical research, rigorous clinical trials, and meticulous data analysis. This careful approach has led to its approval for treating several types of cancer, although ongoing research continually expands its potential applications. The drug’s success reflects a growing understanding of the intricate relationship between the immune system and cancer development.
Understanding Durvalumab’s role requires appreciating the shift towards personalized medicine. This means tailoring treatment to a patient’s unique genetic makeup and disease characteristics. While Durvalumab shows great promise, its effectiveness can vary depending on the specific cancer type, stage, and individual patient factors. Therefore, close monitoring and careful consideration of individual patient needs are critical aspects of treatment.
The information presented here aims to provide a comprehensive overview of Durvalumab, highlighting its mechanism of action, clinical applications, side effects, and overall significance in the fight against cancer. Remember, this information should not be considered a substitute for professional medical advice. Always consult with your physician or oncologist for personalized guidance and treatment decisions.
Mechanism of Action: How Durvalumab Works
Durvalumab’s power lies in its ability to unleash the body’s own immune system against cancer. It achieves this by targeting Programmed Death-Ligand 1 (PD-L1), a protein expressed on the surface of some cancer cells and immune cells. PD-L1 acts as a brake on the immune system, preventing T cells (a type of immune cell crucial for attacking cancer) from effectively destroying tumor cells.
Durvalumab is a monoclonal antibody, meaning it’s a highly specific protein designed to bind to PD-L1. By binding to PD-L1, Durvalumab blocks its interaction with Programmed Death 1 (PD-1) receptors found on T cells. This blockage removes the inhibitory signal, allowing T cells to resume their attack on cancer cells.
Think of it like this: PD-L1 is a “stop” signal for T cells. Durvalumab acts like a wrench, turning off that stop signal. This allows the immune system’s natural defenses to effectively target and eliminate cancer cells that would otherwise evade destruction. The result is a targeted and potentially more effective approach than traditional chemotherapy.
It’s important to note that Durvalumab’s effectiveness depends on the presence of PD-L1 on the cancer cells. Not all cancers express PD-L1 at high levels, and therefore, the response to Durvalumab can vary depending on the tumor’s characteristics. This is a key factor in determining its suitability for individual patients.
Clinical Applications: Where Durvalumab Shines
Durvalumab’s clinical applications are expanding as research continues to reveal its efficacy across various cancer types. Its ability to harness the power of the immune system makes it a valuable tool in the fight against several aggressive and difficult-to-treat cancers. While not a cure-all, Durvalumab has demonstrated significant promise in extending survival and improving quality of life for many patients.
One key area where Durvalumab has shown considerable success is in the treatment of non-small cell lung cancer (NSCLC). Specifically, it’s been approved for use in patients with unresectable Stage III NSCLC following chemoradiation therapy, as well as in some cases of metastatic NSCLC. These approvals highlight its potential to improve outcomes in patients who have exhausted other treatment options.
Beyond NSCLC, Durvalumab is also being investigated and in some cases approved for use in other cancers, including urothelial cancer (bladder cancer) and certain types of head and neck cancer. Clinical trials are ongoing to explore its potential in a wider range of cancers, reflecting the ongoing effort to expand its therapeutic benefits.
The ongoing research into Durvalumab’s clinical applications underscores its importance in the field of cancer immunotherapy. Its unique mechanism of action and demonstrated efficacy in several cancer types make it a promising agent for future treatments and therapeutic combinations. This ongoing exploration reflects the dynamic nature of cancer research and the continual search for improved treatments.
Durvalumab in Non-Small Cell Lung Cancer (NSCLC)
Non-small cell lung cancer (NSCLC) represents a significant area where Durvalumab has demonstrated notable clinical benefit. Its use in NSCLC reflects the growing understanding of the role of the immune system in cancer development and progression. The drug’s success in this challenging disease area has offered new hope to patients and underscores the potential of immunotherapy in oncology.
In particular, Durvalumab has shown efficacy in the treatment of unresectable Stage III NSCLC after concurrent chemoradiation therapy (CRT). This setting is particularly challenging, as these tumors are locally advanced and often unresponsive to conventional treatments. Durvalumab’s ability to prolong progression-free survival in this population has been a major clinical achievement.
Furthermore, research is ongoing to explore Durvalumab’s role in the treatment of metastatic NSCLC. While not yet a standard first-line treatment in all cases, Durvalumab is being investigated in various combination therapies and clinical trial settings to determine its potential for improving outcomes for patients with advanced disease. The results of these trials are eagerly anticipated by oncologists and patients alike.
The use of Durvalumab in NSCLC illustrates the evolving landscape of cancer therapy. It highlights the shift towards a more personalized approach, where treatments are tailored to the specific characteristics of the tumor and the patient’s overall health. The continued research in this area promises further advancements in the treatment of NSCLC.
Stage III NSCLC
Durvalumab has demonstrated significant impact in the treatment of patients with unresectable Stage III NSCLC (non-small cell lung cancer). This stage of the disease presents a considerable challenge, as the cancer is locally advanced but not surgically removable. Traditional treatments often involve concurrent chemoradiation therapy (CRT), but unfortunately, many patients experience disease recurrence.
The pivotal PACIFIC trial showed that Durvalumab, administered after CRT, substantially improved outcomes for these patients. This landmark study demonstrated a statistically significant increase in progression-free survival (PFS) compared to a placebo group. This means patients receiving Durvalumab lived longer without their cancer progressing. The improved PFS translated into a tangible improvement in overall survival, providing a significant clinical benefit.
This success underscores Durvalumab’s ability to target and eliminate residual cancer cells that might remain after CRT. By reactivating the immune system’s anti-tumor response, Durvalumab helps prevent disease recurrence and extends the time patients remain cancer-free. This post-CRT maintenance therapy has become a significant advancement in the management of Stage III NSCLC.
The results from the PACIFIC trial have reshaped treatment guidelines for Stage III NSCLC, establishing Durvalumab as a standard of care following CRT. This success story highlights the transformative potential of immunotherapy and its ability to improve survival rates in patients with advanced-stage cancers who previously had limited treatment options.
Metastatic NSCLC
The treatment landscape for metastatic non-small cell lung cancer (NSCLC) is complex and challenging. Metastatic disease signifies that the cancer has spread beyond the lungs, making it significantly harder to treat. Durvalumab is being actively investigated in this context, often in combination with other therapies, to potentially improve outcomes for these patients.
While not currently a first-line treatment for all metastatic NSCLC patients, Durvalumab is showing promise in specific patient populations and treatment combinations. Clinical trials are exploring its use in combination with chemotherapy regimens, aiming to enhance the effectiveness of conventional treatments and potentially improve overall survival. These trials are carefully designed to assess the safety and efficacy of these combination approaches.
The exploration of Durvalumab in metastatic NSCLC highlights the ongoing effort to develop more effective and targeted therapies for this aggressive disease. Researchers are investigating the drug’s potential in various combinations and patient subgroups to identify the optimal treatment strategies. The results of these ongoing studies are crucial in refining treatment guidelines and improving patient care.
The use of Durvalumab in metastatic NSCLC represents a dynamic and evolving area of cancer research. The ongoing clinical trials and studies are crucial in determining its precise role in improving the outcomes for patients facing this significant challenge. This continuous investigation is a testament to the commitment to improving the lives of those affected by this aggressive form of cancer.
Durvalumab in Urothelial Cancer
Durvalumab’s clinical utility extends beyond lung cancer, showcasing its effectiveness in treating urothelial cancer, which primarily affects the bladder but can also involve the ureters and kidneys. This cancer type often presents significant challenges, emphasizing the need for innovative and effective treatment strategies. Durvalumab offers a novel approach leveraging the body’s immune system to combat the disease.
In the realm of urothelial cancer, Durvalumab has demonstrated clinical activity in both locally advanced and metastatic settings. Its use has been explored in various clinical trials, often in combination with chemotherapy or other immunotherapies, aiming to optimize treatment outcomes and improve patient survival. These trials meticulously evaluate the safety and effectiveness of these different treatment combinations.
The ongoing research into Durvalumab’s role in urothelial cancer reflects the broader shift towards immunotherapy in oncology. The drug’s ability to enhance the immune system’s response against cancer cells makes it a promising agent in this challenging disease area. The results of these trials are crucial in shaping future treatment guidelines and providing better options for patients with urothelial cancer.
Durvalumab’s application in urothelial cancer exemplifies the evolving strategies in cancer treatment. The focus is shifting towards personalized approaches, utilizing a combination of therapies to target the unique characteristics of each patient’s tumor and overall health. The continued research and clinical trials are critical in advancing the treatment of urothelial cancer and improving patient outcomes.
Side Effects and Safety Profile: Understanding the Risks
While Durvalumab offers significant therapeutic potential, it’s crucial to understand its potential side effects. Like many cancer therapies, Durvalumab can cause adverse events, although the severity and frequency vary among patients. Open communication with your healthcare provider is essential to manage any side effects that may arise during treatment.
Common side effects associated with Durvalumab often involve the immune system. These can include fatigue, pneumonitis (lung inflammation), hepatitis (liver inflammation), colitis (inflammation of the colon), and various skin reactions. The severity of these side effects can range from mild to severe, requiring careful monitoring and appropriate management strategies.
Less common, but potentially more serious, side effects can also occur. These may include autoimmune disorders affecting various organs. Regular check-ups and close monitoring by your healthcare team are essential to promptly identify and address any serious complications. Early detection and intervention are key to minimizing the risk of severe adverse events.
It’s vital to remember that the benefits of Durvalumab must be carefully weighed against its potential risks. Your oncologist will assess your individual health status and disease characteristics to determine whether the potential benefits outweigh the risks. This personalized assessment is critical in making informed treatment decisions.
Pros of Durvalumab
Durvalumab offers several key advantages in the fight against cancer. Its unique mechanism of action, targeting the PD-L1 pathway, allows it to harness the power of the patient’s own immune system to combat cancer cells. This targeted approach can lead to more effective cancer cell destruction with potentially fewer side effects compared to traditional chemotherapy.
Clinical trials have demonstrated that Durvalumab can significantly improve progression-free survival (PFS) in specific cancer types, particularly in non-small cell lung cancer (NSCLC) following chemoradiation. This means patients treated with Durvalumab experience a longer period without their cancer progressing, improving their quality of life and overall prognosis. This improved PFS often translates into a longer overall survival time.
Furthermore, Durvalumab’s relatively manageable side effect profile, compared to some other cancer therapies, is a significant advantage. While side effects can occur, they are often manageable with appropriate medical care. This improved tolerability can enhance a patient’s ability to complete the full course of treatment, maximizing the potential benefits of the therapy.
The continued research and development surrounding Durvalumab highlight its ongoing contribution to cancer treatment. Its use in combination therapies and its exploration across various cancer types demonstrate its adaptability and potential to benefit a wide range of patients. This ongoing investigation reflects the dynamism of cancer research and the hope for improved treatment outcomes.
A Promising Future for Immunotherapy
Cons of Durvalumab
While Durvalumab offers significant benefits, it’s essential to acknowledge its potential drawbacks. Like all medications, it carries the risk of side effects, and it’s crucial to discuss these potential risks with your doctor before starting treatment. Understanding these potential downsides allows for informed decision-making and proactive management strategies.
One significant consideration is the potential for immune-related adverse events (irAEs). These side effects arise because Durvalumab stimulates the immune system, which can sometimes mistakenly attack healthy tissues. These irAEs can manifest in various organs, including the lungs (pneumonitis), liver (hepatitis), and intestines (colitis), and can range in severity from mild to life-threatening. Careful monitoring is necessary to detect and manage these events.
Furthermore, Durvalumab’s effectiveness is not guaranteed for all patients. The response to the drug can vary depending on individual factors, such as the specific type and stage of cancer, and the patient’s overall health. Not all patients will experience the same level of benefit, and some may not respond to the treatment at all. This variability underscores the importance of personalized medicine and careful patient selection.
Finally, the cost of Durvalumab can be a significant factor for some patients. The high cost of immunotherapy treatments can pose a financial barrier to access, highlighting the need for insurance coverage and financial assistance programs to ensure equitable access to these potentially life-saving therapies. Open discussion about these financial aspects with your healthcare team is vital.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Elizabeth Dennis, MD [Medical reviewer]
Elizabeth Dennis, MD [Medical reviewer]Dr. Elizabeth Dennis is a highly skilled Orthopedic Surgeon and consultant for RxPulsar.com, a licensed online pharmacy. She specializes in the management and surgical treatment of knee, shoulder, and...
View all posts