No products in the cart.
Over 7,500 medications in stock!
100% Original medicines of Russian and world brands
Fast international shipping and delivery!
Free shipping order $150
24/7 Customer support
Shopping cart (0)
Subtotal: $0.00
Spend $150.00 to get free shipping Congratulations! You've got free shipping.
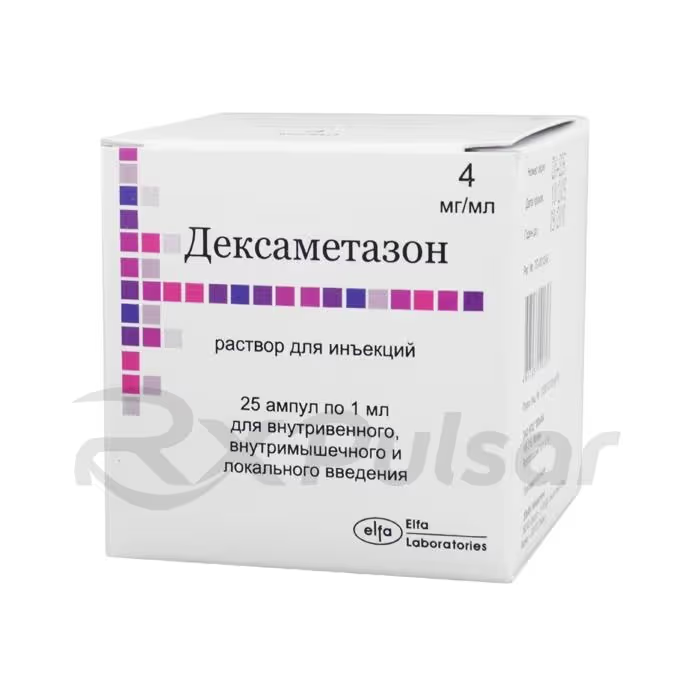
DEXAMETHASONE injection solution 4mg/ml (1ml), 25pcs
🔥 10 items sold in last 3 hours
11 people are viewing this product
Buy from 5 to 10 items and get 2% OFF
on each productBuy from 11 to 30 items and get 5% OFF
on each productBuy from 31 to 100 items and get 10% OFF
on each productBuy from 101 to ∞ items and get 15% OFF
on each productProduct with a Long Shelf Life
100% Original Product
Fast Worldwide Shipping
All forms of DEXAMETHASONE
Analogs of DEXAMETHASONE
Table of Contents
DEXAMETHASONE 4mg Solution 1ml 25pcs Buy Online
Dexamethasone Injection: A Comprehensive Overview
Dexamethasone, a potent corticosteroid, plays a crucial role in managing a wide array of inflammatory and allergic conditions. Its injectable form offers rapid relief when oral administration isn’t feasible or sufficiently effective. This overview explores the key aspects of dexamethasone injection, focusing on its uses, administration, and potential benefits and drawbacks.
What is Dexamethasone?
Dexamethasone is a synthetic corticosteroid, mimicking the actions of cortisol, a hormone naturally produced by the adrenal glands. It exerts powerful anti-inflammatory and immunosuppressive effects, reducing swelling, redness, and allergic reactions. This makes it valuable in treating various severe conditions.
Dexamethasone injection finds application in diverse medical settings. It’s frequently used to treat severe allergic reactions, inflammatory conditions affecting joints and soft tissues, and certain types of edema. Additionally, it can be employed in managing conditions such as asthma exacerbations and certain blood disorders.
The administration route and dosage of dexamethasone injection vary greatly depending on the specific condition being treated and patient factors. It can be administered intravenously (IV), intramuscularly (IM), intra-articularly (directly into a joint), or intralesionally (directly into a lesion). Dosage is determined by a healthcare professional based on individual needs.
Dexamethasone is a long-acting corticosteroid. While elimination from the body typically takes around 20 hours, its effects can persist for several days after the last dose. Factors such as age and other medications can influence its pharmacokinetics and excretion.
The active ingredient is dexamethasone sodium phosphate. Inactive ingredients vary depending on the formulation but may include sodium sulfite, sodium citrate, benzyl alcohol (preservative), and water for injection. Always consult the product information for a complete list of ingredients.
- Rapid onset of action: Provides quick relief from symptoms.
- Potent anti-inflammatory effects: Effectively reduces inflammation and swelling.
- Versatility: Can be administered via various routes depending on the condition.
- Effective in severe cases: Useful when oral medication is insufficient.
- Potential for side effects: Including increased blood sugar, fluid retention, and mood changes.
- Immunosuppression: Can increase the risk of infections.
- Not suitable for all patients: Contraindicated in certain conditions such as infections and peptic ulcers.
- Requires medical supervision: Dosage and administration should be carefully managed by a healthcare professional.
Clinical Use and Indications
Dexamethasone injection is indicated for a wide spectrum of conditions, including: severe allergic reactions, inflammatory disorders (arthritis, bursitis, tendonitis), cerebral edema, certain types of shock, and as adjunctive therapy in various other illnesses. Its use is always guided by a healthcare professional based on individual needs.
Dexamethasone injection is available under various brand names globally. The specific brands and formulations available may vary depending on location and regulatory approvals. Always consult a healthcare provider for information regarding availability in your area.
What is Dexamethasone?
Dexamethasone is a potent synthetic glucocorticoid, a type of corticosteroid. It’s a powerful anti-inflammatory medication that closely mimics the effects of cortisol, a hormone naturally produced by the body’s adrenal glands. This synthetic version, however, offers a more targeted and controlled therapeutic effect, making it invaluable in managing a wide array of inflammatory and allergic conditions. Unlike some other corticosteroids, dexamethasone exhibits a relatively longer duration of action, which contributes to its efficacy in treating severe or chronic conditions.
The mechanism of action involves binding to intracellular receptors, influencing gene expression and ultimately suppressing the inflammatory cascade. This leads to a reduction in swelling, redness, pain, and other symptoms associated with inflammation. Its immunosuppressive properties also make it useful in managing certain immune-mediated diseases where an overactive immune response is a primary driver of pathology. Dexamethasone’s versatility extends to its various routes of administration, allowing for tailored treatment based on individual needs and the severity of the condition.
Clinically, dexamethasone’s impact is significant. It effectively reduces inflammation in various tissues and organs. Its versatility allows for its use in conditions ranging from allergic reactions and asthma exacerbations to more serious illnesses requiring potent anti-inflammatory or immunosuppressive interventions. Understanding its potent effects and potential side effects is crucial for safe and effective utilization.
Uses of Dexamethasone Injection
Dexamethasone injection, due to its rapid onset and potent anti-inflammatory action, finds widespread application across various medical specialties. Its versatility allows for treatment of conditions where oral administration is either impractical or insufficiently effective. The injectable form ensures quicker absorption and higher bioavailability, providing rapid relief in emergency situations and severe cases.
Specific uses frequently include the management of severe allergic reactions, such as anaphylaxis, where immediate intervention is crucial. It’s also commonly employed in treating inflammatory conditions affecting joints and soft tissues, offering significant pain relief and reduction of swelling. Furthermore, dexamethasone injection plays a vital role in managing certain types of edema (fluid retention), particularly in cases of cerebral edema where rapid reduction of swelling is paramount to prevent neurological damage.
Beyond these common applications, dexamethasone injection finds utility in a broader spectrum of conditions. These include, but are not limited to, the treatment of certain types of asthma exacerbations, inflammatory bowel disease flares, and various blood disorders. In some instances, it’s used as adjunctive therapy alongside other treatments to enhance their effectiveness. Always consult with a healthcare professional to determine the appropriateness of dexamethasone injection for a specific condition.
The choice of administration route (intravenous, intramuscular, intra-articular, or intralesional) depends heavily on the specific condition and the location requiring treatment. Healthcare professionals carefully consider these factors when deciding the optimal method for administering dexamethasone injection to maximize its therapeutic benefit while minimizing potential side effects. The dosage is also tailored to the individual patient’s needs and the severity of their condition.
Administration and Dosage
Dexamethasone injection’s administration and dosage are highly variable, tailored to the specific condition, patient factors, and the healthcare professional’s clinical judgment. It’s crucial to understand that self-medication is dangerous; dosages must always be determined and overseen by a qualified medical practitioner. Improper use can lead to serious adverse effects.
The drug can be administered via several routes, each offering distinct advantages depending on the clinical scenario. Intravenous (IV) administration provides rapid systemic effects, ideal for emergencies or conditions requiring immediate impact. Intramuscular (IM) injection offers a slightly slower onset but still provides effective systemic delivery. For localized inflammation, intra-articular (directly into a joint) or intralesional (directly into a lesion) injections may be used, targeting the affected area more precisely.
Dosage regimens vary significantly depending on the indication. In some cases, a single dose might suffice, while others may necessitate multiple doses over a period of days or weeks. Factors like the severity of the condition, the patient’s age, weight, and overall health status all influence the dosage decision. Initial doses may be higher, followed by gradual tapering as the condition improves. Close monitoring is essential throughout the treatment course to adjust the dosage as needed and to detect potential side effects promptly.
Furthermore, the interaction with other medications is a crucial consideration. Concomitant use of certain drugs can affect dexamethasone’s metabolism and efficacy, requiring careful dosage adjustments. Healthcare professionals must carefully consider all these factors to optimize treatment and minimize the risk of adverse events. Always follow the prescribed dosage and administration guidelines meticulously.
Pharmacokinetics and Excretion
Understanding the pharmacokinetic profile of dexamethasone is crucial for effective and safe use. After administration, dexamethasone is rapidly absorbed into the bloodstream, with the rate depending on the route of administration. Intravenous injection, for instance, results in near-immediate systemic distribution, while intramuscular injection shows a slightly delayed absorption. This rapid absorption contributes to dexamethasone’s quick onset of action, a key advantage in managing acute inflammatory conditions.
Once in the bloodstream, dexamethasone binds extensively to plasma proteins, primarily albumin. This protein binding influences its distribution throughout the body, affecting the concentration in various tissues and organs. Dexamethasone readily crosses the blood-brain barrier, explaining its efficacy in treating conditions like cerebral edema. It also crosses the placental barrier, a consideration for pregnant women. The extent of tissue distribution and the concentration in specific organs are influenced by multiple factors including protein binding, blood flow, and the presence of other medications.
Dexamethasone is primarily metabolized in the liver, undergoing extensive hepatic biotransformation into inactive metabolites. These metabolites are then excreted primarily through the kidneys in the urine, with a smaller portion eliminated in the feces. The elimination half-life is relatively long, typically ranging from 3 to 5 hours, meaning that the effects of a single dose can persist for a considerable duration. This extended half-life allows for less frequent dosing, contributing to patient convenience and improved adherence to treatment regimens. However, this also necessitates careful consideration when adjusting dosages and managing potential side effects.
The rate of elimination can be influenced by factors such as age, liver and kidney function, and interactions with other medications. Patients with impaired liver or kidney function may experience slower clearance rates, potentially necessitating dosage adjustments to prevent accumulation and the risk of adverse effects. This highlights the importance of careful monitoring and individualized treatment approaches in managing patients receiving dexamethasone therapy.
Active and Inactive Ingredients
Dexamethasone injection, like all pharmaceutical preparations, contains both active and inactive components. The active ingredient is dexamethasone sodium phosphate, a water-soluble salt of dexamethasone that facilitates rapid absorption and distribution following injection. This specific salt form is chosen for its enhanced solubility and bioavailability compared to other forms of dexamethasone. The concentration of the active ingredient is precisely controlled to ensure consistent and effective dosing.
The inactive ingredients serve various purposes, primarily to stabilize the formulation, ensure its sterility, and enhance its delivery. These excipients, while not therapeutically active themselves, play a vital role in maintaining the integrity and effectiveness of the medication. Common inactive ingredients in dexamethasone injection formulations may include preservatives (such as benzyl alcohol), buffers (to maintain the appropriate pH), and antioxidants (to prevent degradation). The exact composition of the inactive components can vary slightly depending on the manufacturer and specific formulation.
It’s crucial to understand that the inactive ingredients, while generally considered safe, can occasionally cause allergic reactions in sensitive individuals. Patients with known allergies to any of the listed excipients should inform their healthcare provider before receiving the injection. The complete list of active and inactive components should always be reviewed on the product label or package insert to check for potential allergens or other contraindications. Detailed information on the specific inactive ingredients is usually provided by the manufacturer to assist healthcare professionals and patients in making informed decisions.
The precise formulation, and therefore the list of inactive ingredients, may differ across various manufacturers. Consulting the specific product information provided by the manufacturer is therefore vital for patients and clinicians alike. This ensures that any potential interactions or allergic reactions are identified and managed effectively, maximizing the safety and efficacy of the treatment. This attention to detail is paramount in ensuring patient well-being.
Pros of Dexamethasone Injection
Dexamethasone injection offers several key advantages, making it a valuable therapeutic option in various clinical settings. Its rapid onset of action is a significant benefit, providing quicker relief from symptoms compared to oral formulations or other slower-acting treatments. This rapid response is particularly crucial in managing acute conditions requiring immediate intervention, such as severe allergic reactions or life-threatening inflammatory processes. The speed of effect allows for faster symptom control and improved patient outcomes.
The potent anti-inflammatory effects of dexamethasone are well-established. It effectively reduces swelling, redness, pain, and other hallmarks of inflammation, offering substantial symptomatic relief for patients. This potent action is particularly beneficial in managing conditions characterized by significant inflammation, such as acute exacerbations of chronic inflammatory diseases or severe allergic reactions. The ability to target and reduce inflammation is a key driver of its efficacy.
Another advantage lies in the versatility of administration. Dexamethasone injection can be administered intravenously, intramuscularly, intra-articularly, or intralesionally, allowing for targeted delivery depending on the specific clinical need. Intravenous administration is ideal for systemic effects, while intra-articular injection allows for localized treatment of joint inflammation. This flexibility makes it adaptable to a wide range of conditions and treatment approaches.
Finally, dexamethasone injection proves particularly useful in situations where oral administration is impractical or ineffective. This might be due to factors such as severe nausea and vomiting, impaired swallowing, or the need for a more rapid onset of action than oral medications can provide. In such cases, the injectable form provides a valuable alternative, ensuring patients receive the necessary treatment when oral routes are not feasible. This ensures consistent therapeutic benefits even in challenging circumstances.
Brand Names and Availability
Cons of Dexamethasone Injection
While dexamethasone injection offers significant therapeutic benefits, it’s crucial to acknowledge potential drawbacks. One major concern is the risk of adverse effects, which can vary in severity and frequency depending on the dosage, duration of treatment, and individual patient factors. Common side effects include increased blood sugar levels (hyperglycemia), fluid retention (edema), and mood changes (ranging from mild irritability to more serious psychiatric disturbances). These effects often necessitate careful monitoring and may require adjustments to the treatment plan.
Dexamethasone’s potent immunosuppressive properties represent another significant consideration. By suppressing the immune system, dexamethasone increases the susceptibility to infections. This risk is particularly relevant in patients with pre-existing immune deficiencies or those undergoing other immunosuppressive therapies. Careful assessment of the patient’s immune status and prophylactic measures against infections are therefore crucial aspects of safe dexamethasone use.
Furthermore, long-term use of dexamethasone can lead to more serious consequences, including adrenal suppression, osteoporosis, and increased risk of gastrointestinal complications such as peptic ulcers. This highlights the importance of using dexamethasone only when clearly indicated and for the shortest duration necessary to achieve therapeutic benefit. Careful monitoring and gradual tapering of the dose are essential to minimize these long-term risks.
Finally, dexamethasone injection, like any injectable medication, carries a risk of local reactions at the injection site. These can range from mild discomfort and redness to more severe reactions such as pain, swelling, or infection. Proper aseptic technique during injection is essential to minimize this risk. Patients should be aware of these potential side effects and report any concerning symptoms to their healthcare provider immediately.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 David J Bronster, MD [Medical reviewer]
David J Bronster, MD [Medical reviewer]Dr. David J. Bronster, MD, is a distinguished Professor of Neurology and Neurological Consultant to the Recanati/Miller Transplantation Institute. With an impressive 36-year career in consultative wor...
View all posts
Be the first to review “DEXAMETHASONE injection solution 4mg/ml (1ml), 25pcs” Cancel reply


Reviews
There are no reviews yet.