No products in the cart.
Table of Contents
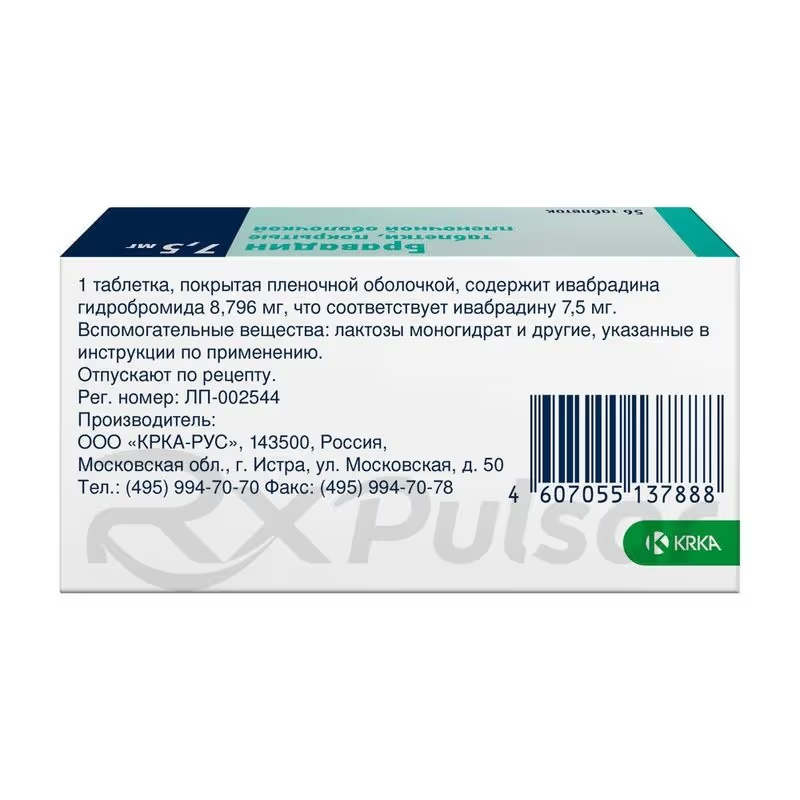
BRAVADIN™ 7.5mg 56 Tablets Buy Online
Bravadin Tablets: A Comprehensive Overview
Experiencing the debilitating symptoms of stable angina? Bravadin, with its unique mechanism of action, may offer significant relief. This comprehensive overview will explore the key aspects of Bravadin 7.5mg tablets, providing valuable insights into its use and potential benefits.
Bravadin 7.5mg tablets are a potent antianginal medication, specifically designed to address the symptoms associated with stable angina pectoris. Its efficacy stems from a precise mechanism targeting the heart’s rhythm, offering a targeted approach to symptom management.
Understanding the precise workings of this medication is crucial for optimal patient care. The selective inhibition of If channels in the sinus node is the cornerstone of Bravadin’s action. This unique mechanism directly influences the heart rate, reducing the frequency of angina episodes.
Understanding Bravadin
Bravadin 7.5mg tablets are a selective If inhibitor, a unique class of antianginal medication. Unlike beta-blockers or nitrates, Bravadin works by specifically targeting the If channels in the heart’s sinus node. This precise mechanism of action leads to a reduction in heart rate, thereby alleviating the symptoms of stable angina.
The reduction in heart rate achieved with Bravadin is generally modest and well-tolerated by most patients. This targeted approach minimizes the potential for significant side effects often associated with other antianginal therapies. It’s important to note that Bravadin is not indicated for the treatment of arrhythmias; its primary application lies in managing the symptoms of stable angina.
Effective management of stable angina requires a multifaceted approach, often incorporating lifestyle modifications alongside medication. Bravadin can be a cornerstone of this strategy, providing significant relief and improving the quality of life for patients suffering from this condition. Individual patient response to Bravadin can vary, and close monitoring by a healthcare professional is essential to optimize treatment.
Before initiating Bravadin therapy, a thorough assessment of the patient’s overall health is crucial. This includes a review of their medical history, current medications, and potential contraindications. The physician should carefully consider the patient’s individual needs and risk factors when prescribing Bravadin.
Mechanism of Action
Bravadin’s therapeutic effect hinges on its unique ability to selectively inhibit the funny current (If) channels located within the sinus node of the heart. These If channels play a crucial role in regulating the heart’s spontaneous rhythm and rate. By blocking these channels, Bravadin effectively slows down the rate at which the sinus node generates electrical impulses.
This reduction in the heart rate, a key characteristic of Bravadin’s mechanism, is achieved without significantly affecting other cardiac functions. This selective targeting minimizes the risk of undesirable side effects often associated with broader-acting antianginal medications. The result is a decrease in myocardial oxygen demand, leading to a reduction in angina symptoms.
The precise modulation of the heart rate by Bravadin contributes to its efficacy in managing stable angina. By slowing the heart rate, Bravadin reduces the workload on the heart, thereby lessening the frequency and intensity of angina episodes. This targeted approach represents a significant advancement in the treatment of stable angina.
Importantly, Bravadin’s mechanism is distinct from that of beta-blockers. While both reduce heart rate, Bravadin achieves this effect through a different pathway, offering a valuable alternative for patients who may not tolerate or benefit from beta-blocker therapy. This distinction underscores the importance of individualized treatment plans tailored to each patient’s specific needs and responses.
Dosage and Administration
The recommended starting dose of Bravadin is typically 5 mg twice daily. This dosage should be carefully considered in conjunction with the patient’s overall health and potential interactions with other medications. Adjustments to the dosage may be necessary based on individual responses and clinical assessments.
After a two-week period of treatment at the initial dose, the physician may increase the dosage to 7.5 mg twice daily, provided the resting heart rate remains consistently above 60 beats per minute. This titration allows for personalized optimization of therapy, ensuring both efficacy and safety.
It is crucial to emphasize that the 7.5 mg tablets are not divisible. Precise dosing is essential, and careful adherence to the prescribed regimen is vital for achieving optimal therapeutic outcomes. Patients should always follow their physician’s instructions precisely.
Regular monitoring of the patient’s heart rate and blood pressure is essential throughout the course of treatment. These vital signs provide valuable insights into the effectiveness of the medication and any potential adverse effects. Adjustments to the dosage may be necessary based on these clinical observations.
Indications and Contraindications
Bravadin is primarily indicated for the symptomatic treatment of chronic stable angina in adult patients with a normal sinus rhythm. This means it’s effective in managing the chest pain associated with this condition, but it’s crucial to remember that it doesn’t address the underlying cause of the angina.
Before prescribing Bravadin, healthcare professionals must carefully consider potential contraindications. These include patients with a history of sick sinus syndrome, sinoatrial block, or second- or third-degree atrioventricular block, unless a pacemaker is in place. The medication is also contraindicated in patients with severe heart failure or hypotension.
Furthermore, Bravadin is not recommended for patients with severe hepatic impairment or those with a known hypersensitivity to ivabradine or any of the tablet’s excipients. Caution should be exercised when prescribing Bravadin to patients with moderate hepatic impairment, necessitating careful monitoring and potential dosage adjustments.
The use of Bravadin should be approached cautiously in patients with certain other conditions, including bradycardia, uncontrolled hypertension, or those taking specific medications that interact with Bravadin. A comprehensive evaluation of the patient’s medical history and current medication regimen is crucial before initiating treatment with Bravadin.
Potential Side Effects
While generally well-tolerated, Bravadin can cause certain side effects, although not everyone experiences them. The most commonly reported side effects are typically mild and transient. However, patients should be aware of these possibilities and report any concerning symptoms to their healthcare provider immediately.
Some of the more frequently observed side effects include bradycardia (slow heart rate), dizziness, and visual disturbances such as blurred vision or luminosity phenomena (phosphenes). These effects are usually dose-related, meaning they may be more pronounced at higher dosages. Careful monitoring of the patient’s heart rate and any visual symptoms is therefore essential.
Less common side effects may include headache, nausea, constipation, and fatigue. The severity and frequency of these side effects vary considerably among individuals. Most are mild and resolve spontaneously, without the need for any intervention. In some cases, dosage adjustments or discontinuation of treatment may be necessary.
Rare but potentially serious side effects can occur, although they are uncommon. These include atrioventricular block and atrial fibrillation. Should any of these serious side effects occur, immediate medical attention is crucial. Patients should be informed about the potential for such side effects and instructed to seek medical advice promptly if they occur.
Pros
Bravadin offers several key advantages in the management of stable angina. Its unique mechanism of action, targeting the If channels in the sinus node, allows for a targeted reduction in heart rate without significantly impacting other cardiac functions. This selectivity minimizes the risk of some side effects associated with other antianginal medications.
Many patients find that Bravadin provides effective relief from angina symptoms, improving their quality of life and allowing them to engage in more physical activity. The targeted approach often leads to a significant reduction in the frequency and intensity of angina attacks, enhancing overall well-being.
The dosage regimen of Bravadin is relatively straightforward, typically involving twice-daily administration. This simplicity can improve patient compliance and contribute to better treatment outcomes. The clear and manageable dosing schedule enhances the ease of integrating Bravadin into a patient’s daily routine.
Furthermore, Bravadin may be a suitable option for patients who cannot tolerate or do not respond well to other antianginal therapies, such as beta-blockers or nitrates. Its distinct mechanism of action provides an alternative treatment strategy, offering a chance for improved symptom control in those who haven’t found adequate relief with other medications. This alternative approach expands treatment options for patients with stable angina.
Cons
While Bravadin offers significant benefits, potential drawbacks should be considered. One notable aspect is the possibility of bradycardia (slow heart rate), a common side effect that necessitates careful monitoring of the patient’s heart rate throughout treatment. This risk underscores the importance of regular clinical assessments.
Another potential drawback is the occurrence of visual disturbances, such as blurred vision or the perception of bright flashes of light (phosphenes). These visual side effects can impact a patient’s daily activities and should be reported to their physician. In some cases, dosage adjustments may be necessary to manage these visual disturbances.
Furthermore, Bravadin is not suitable for all patients with stable angina. Contraindications exist for individuals with certain cardiac conditions, such as sick sinus syndrome or significant heart failure. Careful evaluation of a patient’s medical history is essential before prescribing Bravadin.
Finally, the potential for drug interactions must be considered. Bravadin’s metabolism can be affected by certain medications, necessitating careful consideration of potential interactions when prescribing Bravadin concurrently with other drugs. A thorough review of the patient’s medication list is crucial before initiating treatment.
Important Considerations
Before starting Bravadin, a thorough assessment of the patient’s overall health is paramount. This includes a comprehensive review of their medical history, current medications, and any potential contraindications. The physician should carefully weigh the benefits against the risks for each individual patient.
Regular monitoring of vital signs, particularly the heart rate and blood pressure, is essential throughout the course of treatment. These parameters provide valuable insights into the efficacy and safety of Bravadin therapy, guiding any necessary dosage adjustments. Close monitoring helps optimize treatment and minimize potential adverse events.
Patients should be fully informed about the potential side effects of Bravadin, both common and rare. They should be instructed to report any concerning symptoms, such as significant bradycardia, visual disturbances, or other unusual effects, to their healthcare provider promptly. Open communication is key to ensuring patient safety and effective management.
The possibility of drug interactions should always be carefully considered. Bravadin’s metabolism can be affected by certain medications, highlighting the need for a thorough review of all concurrently used drugs. This comprehensive approach helps prevent unexpected interactions and their potentially adverse consequences. A collaborative approach between the patient and healthcare provider is essential for safe and effective medication management.
Conclusion
Bravadin 7.5mg tablets represent a valuable addition to the therapeutic options available for managing stable angina. Its unique mechanism of action, targeting the If channels in the sinus node, offers a targeted approach to reducing heart rate and myocardial oxygen demand, thereby alleviating angina symptoms. The selective nature of this action minimizes the potential for some of the side effects associated with other antianginal medications.
However, the potential for side effects, such as bradycardia and visual disturbances, necessitates careful patient selection and close monitoring throughout treatment. A thorough understanding of both the benefits and potential risks is crucial for making informed decisions about the use of Bravadin in individual patients. The physician’s role in guiding treatment and monitoring patient response remains paramount.
While Bravadin offers a valuable therapeutic strategy for many patients with stable angina, it’s essential to remember that it is not a cure for the underlying condition. Lifestyle modifications, such as dietary changes and regular exercise, remain crucial components of a comprehensive management plan. A holistic approach, combining medication with lifestyle adjustments, often yields the best outcomes for patients.
Ultimately, the decision to prescribe Bravadin should be made on a case-by-case basis, carefully considering the individual patient’s clinical presentation, medical history, and potential risks and benefits. Close collaboration between the physician and patient is key to ensuring safe and effective treatment.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 David J Bronster, MD [Medical reviewer]
David J Bronster, MD [Medical reviewer]Dr. David J. Bronster, MD, is a distinguished Professor of Neurology and Neurological Consultant to the Recanati/Miller Transplantation Institute. With an impressive 36-year career in consultative wor...
View all posts






Reviews
There are no reviews yet.