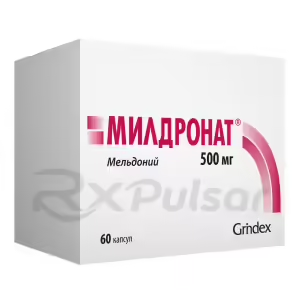
Buy Meldonium
Understanding Meldonium: A Deep Dive into the Active Ingredient
Meldonium, also known as mildronate, has been a subject of both intense interest and controversy. Initially developed in Latvia, its use in sports sparked a global debate, leading to its inclusion on the World Anti-Doping Agency (WADA) prohibited list. However, its potential therapeutic applications continue to be explored, demanding a closer look at its mechanism of action and effects.
The drug’s primary action revolves around its impact on carnitine metabolism. Specifically, it inhibits the synthesis and transport of L-carnitine, a crucial molecule in fatty acid oxidation within cells. This unique mechanism makes meldonium a potential therapeutic tool.
Despite its controversial past, research suggests that meldonium may offer benefits in specific clinical settings. Its ability to modulate energy metabolism in cells could be beneficial in conditions involving ischemia (reduced blood flow), where cellular energy production is compromised. Further research is needed to fully understand its potential.
While generally considered to have a relatively safe profile, meldonium is not without potential side effects. Some reported adverse events include changes in blood pressure, irregular heartbeat, and gastrointestinal disturbances. These side effects, however, are often mild and transient.
The cardiovascular effects of meldonium stem from its influence on cellular energy metabolism. By altering the balance between fatty acid and glucose utilization, it can potentially impact cardiac function. More research is needed to fully elucidate its effects on cardiovascular health.
Meldonium’s neurological effects are another area of ongoing investigation. Preclinical studies hint at potential neuroprotective properties, but human data remains limited. The impact on the central nervous system warrants further examination.
Pros of Meldonium
Potential Benefits
- Potential cardioprotective effects: May help protect the heart from damage in certain conditions.
- Potential neuroprotective effects: Preliminary research suggests possible benefits in neurological disorders.
- Improved exercise tolerance (controversial): Some studies suggest improved performance, but more robust research is needed.
Cons of Meldonium
Potential Risks
- Cardiovascular side effects: Can potentially affect blood pressure and heart rate.
- Neurological side effects: May cause headaches, dizziness, or other neurological symptoms.
- Limited clinical data: More research is needed to fully understand its long-term effects and safety profile.
In conclusion, meldonium remains a fascinating molecule with both promise and controversy surrounding it. While its use in sports has led to restrictions, its potential therapeutic benefits warrant further, rigorous investigation. The currently available evidence indicates that while it may offer some benefits, potential risks also exist, highlighting the need for careful consideration and medical supervision.
Meldonium, a drug initially developed in Latvia, first captured global attention not for its medicinal properties but for its controversial role in professional sports. Its inclusion on the World Anti-Doping Agency’s (WADA) prohibited list in 2016 thrust it into the spotlight, raising questions about its efficacy and safety. This sparked intense debate within the scientific community, prompting a deeper dive into its mechanism of action and potential therapeutic uses.
The story of meldonium is a fascinating blend of scientific advancement, ethical quandaries, and media frenzy. Initially marketed for the treatment of angina pectoris and other cardiovascular conditions, its purported performance-enhancing effects in athletes led to its rapid ban. This ban, however, didn’t halt the ongoing research into its potential applications beyond athletic enhancement.
Understanding meldonium requires navigating a complex landscape of conflicting information. While some studies suggest potential benefits in specific cardiovascular and neurological conditions, the lack of robust, large-scale clinical trials leaves many questions unanswered. Its unique mechanism of action, impacting cellular energy metabolism, presents both opportunities and challenges for its clinical application.
This article aims to provide a comprehensive overview of meldonium, exploring its mechanism of action, reported therapeutic applications, potential side effects, and the ongoing debate surrounding its use. By examining available evidence, we aim to illuminate the complexities of this intriguing substance and its potential role in medicine, while acknowledging the limitations of current knowledge.
The journey to understand meldonium necessitates a careful consideration of both the promising aspects of its potential therapeutic uses and the controversies that have surrounded its application. This exploration will delve into the scientific understanding of its effects on the body, while remaining mindful of the ethical considerations raised by its past association with performance enhancement in sports.
Mechanism of Action: How Meldonium Works
Meldonium’s primary mechanism of action centers around its interaction with carnitine metabolism. Unlike many drugs that directly target specific receptors or enzymes, meldonium subtly influences cellular energy production by interfering with the carnitine shuttle system. This system is vital for transporting long-chain fatty acids into mitochondria, the powerhouses of the cell, where they’re broken down to generate energy (ATP).
By inhibiting the synthesis and transport of L-carnitine, meldonium effectively reduces the amount of fatty acids entering the mitochondria. This shift forces cells to rely more heavily on glucose for energy production. This metabolic switch has significant implications for cellular function, especially under conditions of stress or limited oxygen supply.
The consequences of this metabolic shift are multifaceted and not fully understood. While some researchers suggest that this shift could improve energy production under ischemic conditions (reduced blood flow), others express concern about potential long-term effects of altering cellular energy metabolism. The impact on different tissues and organs remains a subject of ongoing investigation.
It is crucial to note that the precise effects of meldonium depend on various factors, including the dose, duration of treatment, and the specific physiological context. The complex interplay between fatty acid and glucose metabolism makes it challenging to fully predict the consequences of inhibiting the carnitine shuttle. Further research is needed to fully unravel the intricacies of meldonium’s mechanism of action and its broader implications for cellular health.
In essence, meldonium’s mechanism involves a delicate balancing act within cellular energy metabolism. While it might offer benefits in specific circumstances, the potential for unintended consequences necessitates careful consideration and further research to fully understand its long-term effects and ensure its safe and effective use.
Therapeutic Applications: Where Meldonium Shows Promise
While meldonium’s notoriety stems from its association with athletic performance enhancement, research suggests potential therapeutic applications in several areas. Its unique mechanism of action, altering cellular energy metabolism, may offer benefits in conditions where cellular energy production is compromised, such as those involving ischemia (reduced blood flow).
One area of potential application is in cardiovascular disease. Preclinical and some clinical studies suggest that meldonium might have cardioprotective effects by reducing the impact of ischemia on the heart. This protective effect is thought to be related to the drug’s ability to shift cellular energy metabolism towards glucose utilization, reducing the reliance on oxygen-dependent fatty acid oxidation.
Furthermore, there is some evidence suggesting meldonium’s potential in neurological disorders. Its ability to modify cellular energy metabolism could potentially protect brain cells from damage under conditions of reduced blood flow or oxygen deprivation. However, the evidence in this area is still largely preliminary and requires further investigation through robust clinical trials.
It’s crucial to emphasize that the therapeutic applications of meldonium remain largely exploratory. The existing evidence is often based on smaller studies or preclinical models. Larger, well-designed clinical trials are necessary to confirm the drug’s efficacy and safety in these conditions. The results from these studies will be critical in determining its potential role in mainstream medical practice.
In summary, while meldonium shows some promise in treating cardiovascular and neurological conditions, more research is needed to translate these early findings into clinically established therapeutic applications. The existing data highlights the potential, but further investigation is essential to validate these findings and determine its place in clinical practice.
Side Effects: Potential Drawbacks to Consider
While generally considered well-tolerated, meldonium is not without potential side effects. Although many reported adverse events are mild and transient, understanding these potential drawbacks is crucial for informed decision-making. The frequency and severity of side effects can vary depending on factors such as dosage, duration of treatment, and individual patient characteristics.
Some of the more commonly reported side effects include gastrointestinal disturbances such as nausea, vomiting, and diarrhea. These are often mild and typically resolve without intervention. However, in some cases, they may necessitate dose adjustment or discontinuation of the medication. It’s important to monitor for such symptoms and report them to a healthcare provider.
Cardiovascular effects are another area of concern. Changes in blood pressure, both increases and decreases, have been reported. Similarly, alterations in heart rate, including both tachycardia (rapid heart rate) and bradycardia (slow heart rate), have been observed. These cardiovascular effects highlight the need for careful monitoring, especially in individuals with pre-existing heart conditions.
Less frequently reported side effects include neurological symptoms such as headaches, dizziness, and sleep disturbances. Allergic reactions, although rare, are also a possibility. The occurrence of such adverse effects underscores the importance of careful patient selection and close monitoring during treatment. The benefits of meldonium must always be weighed against its potential risks.
In summary, while meldonium appears relatively safe for many individuals, potential side effects, ranging from mild gastrointestinal issues to more significant cardiovascular or neurological events, need careful consideration. Open communication with a healthcare provider is essential for identifying and managing any adverse effects that may arise during treatment.
Cardiovascular Effects: A Closer Look
Meldonium’s impact on the cardiovascular system is a complex area requiring careful consideration. Its primary mechanism of action, altering cellular energy metabolism, can indirectly influence cardiac function. While some studies suggest potential benefits, such as protection against ischemia-induced damage, other findings highlight potential risks, making it crucial to approach this topic with nuance.
The shift in cellular energy metabolism induced by meldonium—a move towards glucose utilization and away from fatty acid oxidation—could theoretically offer protection during periods of reduced blood flow (ischemia). This is because glucose metabolism is less dependent on oxygen compared to fatty acid oxidation. However, the clinical significance of this metabolic shift remains debated.
Conversely, some studies have reported potential adverse cardiovascular effects, such as changes in blood pressure and heart rate. These effects, although often mild, emphasize the need for careful monitoring, particularly in individuals with pre-existing cardiovascular conditions. The potential for interactions with other medications further complicates the picture.
The observed cardiovascular effects are likely a consequence of the drug’s multifaceted influence on cellular processes. The interplay between altered energy metabolism, potential effects on blood vessel tone, and the overall impact on cardiac function necessitates further research to fully understand the complexities of meldonium’s cardiovascular profile. This includes a need for larger, well-controlled clinical trials.
In conclusion, meldonium’s cardiovascular effects are not fully understood and warrant further investigation. While potential benefits in ischemic conditions exist, the possibility of adverse effects, particularly in individuals with pre-existing heart conditions, demands careful monitoring and consideration.
Weighing the Risks and Rewards
Neurological Effects: Impact on the Central Nervous System
Meldonium’s effects on the central nervous system (CNS) are another area of ongoing research, with both potential benefits and risks requiring careful consideration. Its influence on cellular energy metabolism, primarily by altering the balance between glucose and fatty acid utilization, could have implications for neuronal function and survival under conditions of stress or injury.
Some preclinical studies suggest that meldonium might exert neuroprotective effects. By shifting cellular energy metabolism towards glucose, it may help protect neurons from damage caused by ischemia (reduced blood flow) or other forms of cellular stress. This potential neuroprotective action is an area of considerable interest, but requires more robust clinical data.
However, it’s also important to acknowledge the potential for adverse neurological effects. Some individuals have reported side effects such as headaches, dizziness, and sleep disturbances. These side effects, although often mild and transient, highlight the need for careful monitoring, especially in patients with pre-existing neurological conditions.
The exact mechanisms underlying meldonium’s neurological effects are not fully elucidated. The interplay between altered cellular energy metabolism, potential effects on neurotransmitter systems, and the overall impact on neuronal function requires further research. This includes well-designed clinical trials to assess both its potential therapeutic benefits and the frequency and severity of adverse neurological events.
In conclusion, while meldonium’s potential to protect neurons from damage is intriguing, further research is crucial to fully understand its neurological effects. The balance between potential therapeutic benefits and the possibility of adverse neurological events necessitates careful consideration and further investigation.
-
 Georgia Austin [Author]
Georgia Austin [Author]Georgia Austin is a seasoned SEO content writer, editor, and content marketing strategist with over 7 years of experience crafting compelling copy for leading brands in the healthcare and pharmaceutic...
View all posts
-
 Jonathan Brown [Editor]
Jonathan Brown [Editor]Jonathan Brown is a seasoned professional editor, researcher, and educator with over 12 years of experience helping authors find their voice and polish their writing. As a content editor for RxPulsar....
View all posts
-
 Jessica Kerns, MD [Medical reviewer]
Jessica Kerns, MD [Medical reviewer]Dr. Jessica Kerns is a highly accomplished pediatrician and adolescent medicine specialist who serves as a clinical instructor in the Department of Pediatrics at the Icahn School of Medicine at Mount...
View all posts